By Andrea Hayes, MD, F.A.C.E.
It is characterized by high blood sugar levels which, if left unmanaged, can lead to a variety of life-threatening complications, including heart disease, stroke, blindness and kidney failure. We have learned a great deal about the disease and treatments have improved dramatically in recent years. However, the differentiation of Type 1 and 2 diabetes is not always well defined and the disease states can overlap in several ways. As a result, some patients are not provided the proper treatment plan to help them best manage their disease.
Historical Generalizations Drives Misdiagnosis
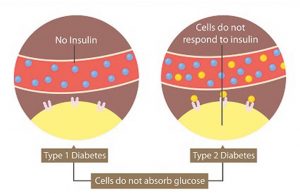
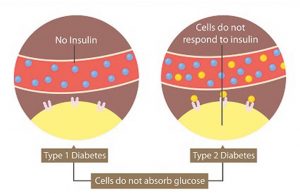
Historically, Type 1 diabetes was considered “children’s diabetes,” based on the belief that Type 1 diabetes primarily affected children and adolescents. Type 2 diabetes was labeled as “adult diabetes” because it was more prevalent among adults. This perception stemmed from observations made by medical professionals based on the age at diagnosis and the underlying causes of each condition. While both forms of diabetes cause high blood sugar levels in patients with the disease, there are fundamental differences between Type 1 and Type 2.
Type 1 Diabetes
Type 1 diabetes, previously referred to as “juvenile diabetes” or “insulin-dependent diabetes,” is an autoimmune disorder where the body’s immune system attacks the islet cells in the pancreas that make insulin. As a result, the pancreas fails to make insulin, leading to elevated blood sugar levels. While it often develops in childhood or adolescence, there has been a rise in adult-onset Type 1 diabetes cases. This phenomenon dispels the notion that it exclusively affects young individuals.
Adult-onset Diabetes Often Misdiagnosed
One form of adult-onset Type 1 diabetes is known as Latent Autoimmune Diabetes in Adults (LADA). LADA shares similarities with Type 2 diabetes in terms of its onset later in life, but it is characterized by an autoimmune response like Type 1 diabetes. LADA is often misdiagnosed as Type 2 diabetes initially, as it progresses more slowly than classical Type 1 diabetes. It is essential for medical professionals to be aware of this distinction to provide appropriate treatment and care.
Type 2 Diabetes
Type 2 diabetes, previously labeled “adult-onset diabetes” or “non-insulin-dependent diabetes,” is the most common form of diabetes. While Type 2 also results in high blood glucose levels, it is due to the body becoming resistant to the effects of insulin and when the pancreas fails to produce enough insulin to maintain normal blood sugar levels. While it is predominantly observed in adults, we are now witnessing an alarming trend of increased Type 2 diabetes cases among younger individuals, partly driven by the obesity epidemic.
The rise in childhood obesity has played a significant role in the increased prevalence of Type 2 diabetes among young people. Unhealthy diets and sedentary lifestyles contribute to weight gain and insulin resistance, increasing the risk of developing this condition. It is crucial to address these lifestyle factors and promote healthier habits to prevent and manage Type 2 diabetes in children.
Challenges in Diagnosis
Differentiating between Type 1 and Type 2 diabetes can be challenging due to overlapping symptoms and atypical presentations. Misdiagnosis can occur, leading to delayed or inadequate treatment. It is important for healthcare providers to consider various factors, including age, family history, body weight, and autoimmune markers to make an accurate diagnosis.
I was recently referred two gentlemen, ages 24 and 46 with similar presentations. Each are very fit and active. They had each been diagnosed with Type 2 diabetes and were taking oral medications appropriate for that diagnosis. Their blood sugars were wildly out of control with sugars ranging above 300 mg/dl often. After confirmatory lab work, I determined that each actually had a form of Type 1 diabetes. I initiated insulin and stopped the oral medications. Their blood sugars dropped to more normal levels and were more easily controlled. Both patients were diagnosed later in life than a typical Type 1 diabetic and have a latent onset of immune-based diabetes. These cases illustrate that the formerly defined classes of diabetes are not universally accurate. Proper diagnosis often requires more exploration, testing and time.
Treating Type 1 and Type 2 Requires Effective Management
Early detection, proper diagnosis, and personalized treatment plans are essential for effectively managing both Type 1 and Type 2 diabetes. For Type 1 diabetes, lifelong insulin therapy is necessary, as the body cannot produce insulin on its own. In Type 2 diabetes, lifestyle modifications such as healthy eating, regular physical activity, and medication may be prescribed to control blood sugar levels.
It is important to note that individuals with diabetes, regardless of the type, can lead fulfilling lives with proper management. Regular blood sugar monitoring, healthy lifestyle choices, and ongoing medical care are crucial components of diabetes management.
If you have any concerns or experience symptoms related to diabetes, consult a healthcare professional for an accurate diagnosis and appropriate treatment.
Andrea Hayes, MD received her Type 1 diagnosis at age 15. She is a board-certified endocrinologist who has been in practice for 25 years. She offers prompt appointments for patients in home, local office or via telehealth.
For more information, call 239-641-8199 or visit: naplesdiabetesconcierge.com
 Southwest Florida's Health and Wellness Magazine Health and Wellness Articles
Southwest Florida's Health and Wellness Magazine Health and Wellness Articles

