By Scott Woolverton, M.D.
 He’s in his 70s now and is feeling the aches and pains that can come with age. But lately, even walking is difficult. Cramping pain in his calves makes him stop, and although the pain subsides as he rests, it just comes back when he moves on. The distance he can walk without pain is becoming shorter and shorter.
He’s in his 70s now and is feeling the aches and pains that can come with age. But lately, even walking is difficult. Cramping pain in his calves makes him stop, and although the pain subsides as he rests, it just comes back when he moves on. The distance he can walk without pain is becoming shorter and shorter.
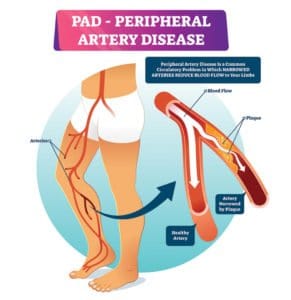
Although fictitious, this case is a classic example of someone with peripheral artery disease, or PAD, a condition that affects as many as 12 million people in the United States, and increases in prevalence with age. One in eight Americans older than 60 years of age have PAD but only 25% of the general population is aware of the disease.
PAD develops when arteries become completely or partially blocked with plaque deposits that limit blood flow to legs. Just like clogged arteries in the heart, clogged arteries in the legs increase the risk of heart attack, stroke or even death.
Atherosclerosis (plaque buildup) in the legs does not always cause symptoms, so many people can have PAD and not know it. People who do experience symptoms, such as pain or cramping in the legs, often do not report them, believing they are a natural part of aging or due to another cause.
While some with PAD do not experience symptoms, people should be aware of certain factors that put
them more at risk. Smokers are four times at greater risk, African Americans are three times more likely to have PAD, and one in every three people over the age of 50 with diabetes is likely to have the disease.
Common risk factors for PAD include high cholesterol, smoking, high blood pressure, diabetes, inactivity, atherosclerosis and age. As many as six million people with diabetes are affected by PAD, making it one of the primary co-morbidities of diabetes.
Chronic toe and foot sores are common in people with PAD, as are cramping, numbness, weakness or heaviness in the leg muscles. Those who have any of the risk factors for PAD should ask their healthcare professional about PAD. A physician can check for signs of the disease with a simple test of pulses in the feet.
PAD also can indicate plaque buildup in other important blood vessels, like those that feed the heart and brain. Frequently, patients diagnosed with PAD also may need studies of cardiac and carotid arteries.
In some severe cases of PAD, surgery may be needed to open arteries that have narrowed. Consult with a physician to see if surgery is a necessary treatment. If so, the surgeon will seek to repair the blockage either during a catheterization with stents and balloons or in the operating room with bypass.
In less severe cases of PAD, lifestyle changes and medication can help to manage the condition. It’s important to gain a complete medical history and understanding of a patient’s lifestyle that can indicate risk factors for PAD.
Gulf Coast Medical Group is offering free screenings for PAD through March 1, 2020. To schedule an appointment with a physician to assess your risk factors, call 844-366-9362.
Action Steps to Help Manage PAD
The Venice Regional Bayfront Health Center for Wound Care recommends the following action steps to help manage PAD:
• Make lifestyle changes, such as quitting smoking and correcting blood pressure and cholesterol numbers.
• Develop healthy eating habits and an exercise plan.
• Exercise regularly to help increase blood circulation and reduce pain in the lower extremities. Walking, hiking and bike riding are good exercise options. A personal trainer can help tailor a custom workout plan that best fits a person’s needs.
• Always consult with a physician about which medications may help PAD and if they are needed.
• See a physician for regular foot exams, which can identify any open sores early.
Scott Woolverton, M.D., is an interventional cardiologist at Gulf Coast Medical Group Heart & Vascular Center.
Venice Regional Bayfront Health
Call 844.366.9362 or visit VeniceRegional.com









