By Lam Nguyen, MD, Orthopaedic Spine Surgeon
Low back pain exacts a significant burden on the healthcare system and is the source of approximately 12 million physician office visits per year in the United States. It is among the leading causes of disability, accounting for expenditures in excess of $50 billion every year. Although nearly 1 million spinal fusions are performed annually, outcomes studies have demonstrated success rates anywhere from 35% to 89%. Therefore, it can be concluded that the etiology of back pain is complex and may originate outside of the spine itself.
There are many different causes of low back pain, and the sacroiliac joint (SI joint) is a source of low back pain. Unfortunately, the SI joint is an under-appreciated and under-diagnosed etiology of chronic axial low back pain. Even in orthopaedic surgery residency training, outside of the trauma setting, the SI joint receives very little attention as part of the formal curriculum. Yet, it is the largest axial joint in the body, and it has been demonstrated that the SI joint is responsible for up to 30% of cases of chronic low back pain, and this number may be even higher in patients who have had lumbar spinal fusion surgery.
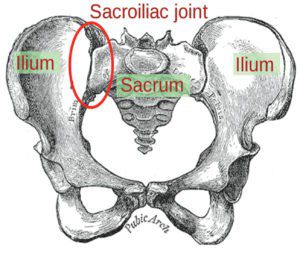
The SI joints are weight-bearing joints. They are the lowest point of the spinal column, and they provide the transition from the spinal axis to the pelvis (Figure 1). The SI joints are critical in the transfer of load from the upper and lower extremities to the pelvis and the lumbar spine. Furthermore, important nerves of the thigh and leg pass in front of the SI joints.
The most common presentation of SI joint dysfunction is low back pain. However, because important nerves of the lower extremity does pass adjacent to the SI joint, irritation/inflammation of the SI joint can affect the nearby nerves and cause buttock, groin, and leg symptoms similar to sciatica.
It is not clearly understood why sacroiliac joint dysfunction occurs. Most cases of SI joint dysfunction are idiopathic (the cause is unknown). However, other sources of pain generation may come from ligamentous instability, altered joint mobility and stress, microfracture, osteoarthritis, infection, and inflammation.
One of the most challenging aspects of treating SI joint pain is the complexity of diagnosis, because SI joint dysfunction can present with symptoms similar to that of a patient with spine or hip problems. Dozens of physical examination tests have been advocated as diagnostic aids in patients with presumed SI joint pain. However, no specific physical examination tests have been validated that accurately identify a painful sacroiliac joint.
No imaging studies consistently provide findings that are helpful to diagnose primary sacroiliac joint pain. Computed tomography (CT), magnetic resonance imaging (MRI), and bone scan are done predominantly to exclude other causes of pain than to diagnose idiopathic SI joint dysfunction.
Because of limitations of the physical examination and imaging modalities, imaging-guided, contrast-enhanced sacroiliac joint injections are the only method for definitively diagnose or exclude the sacroiliac joint as a source of pain. Ideally, for a test to be considered diagnostic, complete relief of the pain emanating from the sacroiliac joint should be achieved. However, published studies have used ≥75% pain relief as diagnostic of sacroiliac joint–mediated pain and ≤50% relief as not diagnostic, with 51% to 74% relief considered equivocal.
If the clinical situation warrants, an apparently positive response should be confirmed with a subsequent control block.
Treatment goals include decreasing pain and improving function by restoring balance in lumbopelvic and hip joint kinematics and function, and establishing core body and lower extremity muscular strength and balance. The patient with SI joint pain is best managed with a multi-disciplinary collaborative approach. Nonsurgical treatment can include medications, physical therapy, activity modification, bracing, chiropractic manipulation, injections, and radio-frequency ablation.

Surgical treatment involves fusion of the affected sacroiliac joint (Figure 2). However, Si joint fusion should be considered only in patients with joint pain proven by controlled diagnostic anesthetic blocks and without any pain sources in the lumbar spine or the hip joints. It also should be reserved for those who have not responded to aggressive conservative care and who have radiographic evidence of SI joint degeneration or destruction. There are many surgical techniques described. Ask your doctor one which technique he/she would recommend for you.
For more information on their services and organization, please visit their website at www.Kwoc.net.
941-893-6447









