By Joseph Gauta, MD, FACOG
 Until recently, pelvic organ prolapse (POP) was rarely addressed because women were reluctant to discuss the embarrassing symptoms. POP is one of the most common disorders women will face in their lifetime. Today, many gynecologists and primary care physicians routinely screen women for symptoms, and a new surgical specialty of urogynecology has arisen to treat pelvic organ prolapse and the incontinence that often accompanies this problem.
Until recently, pelvic organ prolapse (POP) was rarely addressed because women were reluctant to discuss the embarrassing symptoms. POP is one of the most common disorders women will face in their lifetime. Today, many gynecologists and primary care physicians routinely screen women for symptoms, and a new surgical specialty of urogynecology has arisen to treat pelvic organ prolapse and the incontinence that often accompanies this problem.
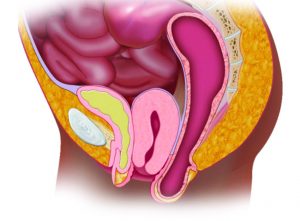
Pelvic organ prolapse is a term used to describe the dropping of a pelvic organ through or out of the vagina. Pelvic organs include the bladder and urethra, the rectum and anus, and of course the uterus and vagina itself. Pelvic organ prolapse is an unfortunately common problem, with childbirth, age, menopause, and hysterectomy being the most common causes and smoking, chronic coughing or heavy lifting, chronic constipation, diabetes, and obesity being common risk factors. POP is expected to affect half of all women and 1 in every 9 will undergo surgical treatment to correct prolapse.
Think of the vagina as though it were an empty pillowcase that can turn inside out in the wash. Prolapse is like the pillow case trying to turn inside out because the support structures of the vagina and pelvis have weakened and are not holding the tissues and organs in place anymore. Anything that can stretch or break these support structures (ligaments and muscles) can cause POP.
Symptoms – Sometimes a patient doesn’t even know she has prolapse until her doctor points it out during her exam. However, many patients experience discomfort with a range of symptoms, including:
Pain and Pressure: lower back discomfort or pressure sensation in the vagina that gets worse by the end of the day or during bowel movements.
Urinary Symptoms: urinary frequency, stress incontinence or difficulty starting to urinate.
Bowel Symptoms: constipation, accidental loss of stool or pressure or pain during bowel movements
Sexual Difficulties: pain with intercourse due to irritated vaginal tissue.
Treatment: Women with mild to no symptoms don’t need treatment, but should avoid risk factors that could worsen the problem such as smoking, lifting heavy weight or being overweight. If you are experiencing major discomfort, POP can be successfully treated using many different modalities, from exercise to medicine to splints (pessaries) to surgery. Let’s summarize these treatments.
• Pelvic Floor Exercises have the advantage of being noninvasive, and in mild cases can help to relieve some symptoms of discomfort or maybe leaking. Prolapse is not reversed using this treatment.
• Medicine, like vaginal estrogen creams, can also alleviate some symptoms, but also do not reverse the prolapse.
• Pessaries are excellent in keeping the pillow case (vagina) from turning inside out by taking up space in the vagina like a pillow does in a pillow case. A pillow case can’t turn inside out if the pillow is in it! Pessaries are great for temporary control of the pro-
lapse or for people who cannot proceed with other treatments. They can provide permanent relief of the symptoms of prolapse, but must be maintained and cleaned periodically.
• Surgery is the treatment for any hernia in the body. With surgery the prolapsed organ will be repositioned and secured to the surrounding tissues and ligaments. When the benefits of surgery outweigh the risks, surgery may be the best choice. Surgery involves anesthesia and recuperation time, but may be the best long term option. All surgeries for POP can be done on an outpatient basis.
If you’ve been diagnosed with POP understanding your treatment options is extremely important. All treatments have their advantages and drawbacks, which should be thoroughly discussed with your urogynecologist before decisions are made. Make sure your urogynecologist is Board Certified and has extensive experience in dealing with your specific problem.
For more information or to make an appointment call, Dr. Joseph Gauta at The Florida Bladder Institute in Naples, Florida at 239-449-7979 or 239-592-1388. www.floridabladderinstitute.com










