 An achy back, incontinence, and pelvic pain may all have one sneaky cause. And your doctor has probably never mentioned it.
An achy back, incontinence, and pelvic pain may all have one sneaky cause. And your doctor has probably never mentioned it.
For a condition so hard to diagnose, Pelvic Floor Disorder, PFD, is surprisingly common. By some estimates, it affects one in three American women. Giving birth boosts your chances of developing a pelvic-floor issue by 18 percent if you’ve had one child and 32 percent if you’ve had three or more.
Hormonal declines in menopause and loss of muscle mass with age are among other culprits for women. Surgery or an accident (like falling on your hip or tailbone) may play a role, as can obesity. In your 50s and 60s, your PFD risk nearly triples, compared with in your 20s or 30s.
Though pelvic floor disorder is less prevalent in men, it’s still underdiagnosed. Some 90 percent of chronic prostate infections, for example, are not caused by bacteria; experts suspect a weak pelvic floor may be a factor. Surgery, injury, obesity, and chronic constipation can damage the pelvic floor in men, leading to incontinence, pain, and problems with sexual performance. Men may be embarrassed to seek treatment—and, like women, they are often misdiagnosed if they do.
For many patients PFD manifests as pain in the vulva. In others, it presents as a bowel disorder; endometriosis; or bladder, hip, back, or abdominal pain. Often, doctors treat symptoms in the affected organ or joint rather than find the real cause. Sometimes, doctors try to treat just the vulva pain, the constipation, or the hip joints. But when you miss the cause, you can’t really fix the problem.
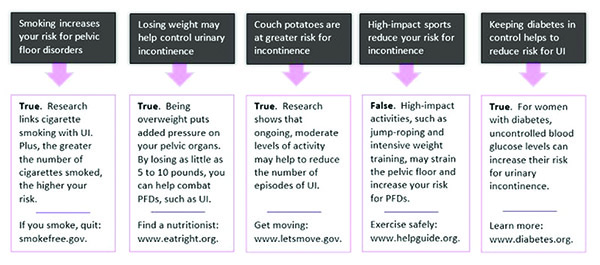
Knowing the risk factors can decrease your chances of experiencing PFD.
The Path to Real Relief
PFD is gaining recognition among pelvic-pain specialists, gastroenterologists, urologists, gynecologists, colorectal doctors, and urogynecologists, who have expertise in both bladder and pelvic health. The first step to relief is a pelvic-floor evaluation, followed by physical therapy.
The exam is a lot like the gloved internal check a gynecologist does, although with more focus on muscle function. The specialist will look for tenderness, pain, and tension in the muscles. Men are diagnosed by a urologist or other specialist after a thorough examination of the groin and a rectal exam.
This should be frontline treatment. If you’re not seeing a specialist who understands the impact these muscles have on pain, you may not be getting the best care. Less than half the women who would benefit from a pelvic-floor evaluation get one.
While there are drugs for and surgical solutions to some pelvic-floor problems, physical therapy plus home routines may help many patients feel better. A 2014 study of nearly 800 women with PFD found that most saw incontinence, constipation, and/or pain improve by at least 80 percent with pelvic-floor physical therapy. In another study, people with lower-back pain got extra relief when they added pelvic-floor exercises to back exercises and ultrasound.
Other treatments include massage-like work inside the vagina by a therapist to release tight spots, with biofeedback to train a patient to tighten and relax the muscles herself. It’s not weird. Treatments are very professional. Patients also do daily exercises at home, including Kegels to strengthen weak muscles and relaxation exercises for tense muscles, hip flexors, and glutes.
Dr. Gauta is now the first physician in S.W. Florida dual board certified in Urogynecology and Obstetrics and Gynecology. Dr. Gauta’s practice, The Florida Bladder Institute, is solely dedicated to Urogynecology. One out of every six women suffers from overactive bladder and half of all women will suffer from pelvic organ prolapse. A challenge for women seeking treatment is that they would go to a urologist for one problem, a gynecologist for another and a gastroenterologist for another. Dr. Gauta explains “A Urogynecologist has the skill and experience to assess the entire pelvic region including the uterus, bladder, vagina, rectum as well as the muscles, ligaments, connective tissue and nerves that support those systems. Evaluating your pelvic system as a whole ensures the best treatment and outcome”. Some of the newer treatment options include biofeedback, electrical stimulation, Botox, and minimally invasive outpatient surgery. In addition to providing the most advanced medical care for his patients, Dr. Gauta is a preceptor for Boston Scientific, Medtronic and Olympus and trains other physicians from around the world on how to do the most advanced Urogynecology procedures. He is the recipient of the prestigious Castle Connolly’s Top Doctors award, and is amongst the top 1% of physicians in the country who are honored with the Patient’s Choice Award for 5 years in a row. Dr. Gauta received his training at Tulane University in New Orleans mentored by world renowned Urogynecologists David Herbert M.D. and Thomas Elkins M.D.
Florida Bladder Institute
239-449-7979
www.FloridaBladderInstitute.com










