By Julian J. Javier, MD – Cardiac and Vascular Specialist
 Varicose veins are a very common condition in the United States and effect as many as 50 percent of adults.
Varicose veins are a very common condition in the United States and effect as many as 50 percent of adults.
For many men and women, varicose veins and spider veins (these are the smaller and more common variation of varicose veins) makes them feel less attractive, and are a cosmetic concern. However, for others, varicose veins cause aching pain and discomfort.
What are Varicose Veins?
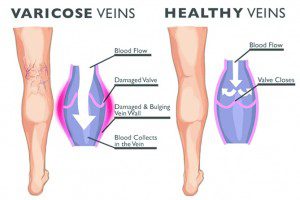
Varicose veins are the blue or purplish enlarged veins you typically see bulging out of one’s leg. Any vein in your body may become varicose; however, varicose veins most often appear in the legs. Varicose veins occur in the legs and lower extremities because standing and walking increases the pressure in the veins in the lower half of your body.
In healthy veins, tiny valves open as blood flows toward your heart and then close to stop blood from flowing backward. In varicose veins, the valves are weakened or damaged allowing blood to flow backward causing swelling and the veins to become damaged.
This condition may lead to serious problems such as Thrombosis (blood clots) or venous stasis ulcers (slow or non-healing sores). Moreover, varicose veins may also indicate that the individual is at higher risk of other disorders of the circulatory system.
Symptoms of Varicose Veins
A number of people do not experience any discomfort with varicose veins, however, some people do. Here are some uncomfortable symptoms common with varicose veins:
• Dark blue or purple veins
• Twisted, thickened veins
• Achiness or heaviness in the legs
• Veins feel like they are burning, throbbing or itchy
• Swelling in the lower legs
• Pain is worse after sitting or standing for long periods of time
• Skin ulcers on the leg and ankle. Skin ulcers can indicate severe vascular disease, and may require immediate attention.
Risk Factors for Varicose Veins
• Standing for long periods of time: Blood doesn’t flow as well if you’re in the same position for long periods of time because your muscles are not contracting to push the blood back to the heart.
• Obesity: Extra weight puts more pressure on your
veins.
• Age: As you age, normal wear and tear weakens vein walls and venous valves which regulates blood flow.
• Sex: Women are more likely than men to develop varicose veins and spider veins. This is attributed to hormonal changes during pregnancy, PMS and menopause. The female hormone estrogen may relax vein walls, and hormone replacement therapy and birth control pills may also increase your risk of varicose veins.
• Genetics: You are more likely to have varicose veins if close family members have them.
• Injury or Trauma to the leg
Varicose Vein Treatment Options
Varicose veins are treated with a combination of lifestyle changes and medical intervention.
Lifestyle changes
Losing weight, eating a balanced diet and engaging in regular exercise can alleviate varicose veins and associated discomfort of pain. If you sit for prolonged periods of time, taking activity breaks will help rev up your circulation.
Doctors usually recommended compression stockings for patients with varicose veins. Full length pantyhose offers the mildest support. Compression garments offer the next level support, and are available in above or below the knee socks or full length compression hose. Your doctor may recommend a prescription level supporting garment, which can usually be purchased from a medical supply store or pharmacy.
Non-Invasive Treatments
If a combination of self-management and compression garments are not sufficient to manage your symptoms, or if you would like to remove them for cosmetic reasons, there are a number of procedures your doctor can use to remove varicose veins:
• Sclerotherapy: One of the most commonly used procedures to remove small varicose veins and spider veins. In this non-surgical procedure your doctor injects a liquid chemical into the vein, which causes irritation and scarring, causing the body to close off the vein and reabsorb it into the body. Sclerotherapy can be done in your doctor’s office and usually does not require anesthesia.
• Endovenous Ablation: Uses laser or radio waves to burn (cauterize) and close off problem veins. This procedure is minimally invasive and most effective on small to medium sized veins. Veins that have been closed off are reabsorbed into the body.
• Ambulatory Phlebectomy: This procedure uses tiny punctures or incisions to remove small portions of the vein, one section at a time. No stitches and little recovery time are expected. The incisions are so small no stitches are required.
• Vein Ligation & Stripping: Older methods of treating veins, ligation includes making small incisions over the problem vein and tying off the vein in order to cut off blood flow, which in turn causes the vein to become less visible. Vein stripping involves tying off of the upper end of a problem vein and then removing the vein. Long veins are often removed this way.
Prevention of Varicose Veins
There’s no way to completely prevent varicose veins. But improving your circulation and muscle tone can reduce your risk of developing varicose veins or getting additional ones. Traditional, common-sense approaches include:
• Exercise. Get your legs moving. Walking is a great way to encourage blood circulation in your legs. Your doctor can recommend an appropriate activity level for you.
• Watch your weight, and your diet. Shedding excess pounds takes unnecessary pressure off your veins. What you eat makes a difference, too. Follow a low-salt, high-fiber diet to prevent the swelling that may result from water retention and constipation.
• Watch what you wear. Avoid high heels. Low-heeled shoes work calf muscles more, which is better for your veins. Don’t wear tight clothes around your waist, legs or groin. Tight panty-leg girdles, for instance, can restrict circulation.
• Elevate your legs. To improve venous circulation, take several short breaks daily to elevate your legs above the level of your heart. For example, lie down with your legs • Avoid long periods of sitting or standing. Make a point of changing your position frequently to encourage blood flow. Try to move around at least every 30 minutes.
• Don’t sit with your legs crossed. This position can aggravate circulation problems.
Julian J. Javier, M.D.
239.300.0586
Julian J. Javier, M.D.
Cardiac and Vascular Specialist
LANGUAGES: English, Spanish, Creole
HOSPITAL PRIVILEGES: Naples Community Hospital
SPECIAL FOCUS: Venous Disorders
BOARD CERTIFICATIONS: Interventional Cardiology, Cardiology, Internal Medicine
MEDICAL SCHOOL: UASD
RESIDENCY: Saint Louis University School of Medicine
FELLOWSHIP: Saint Louis University School of Medicine
ACADEMIC APPOINTMENTS: University of Miami School of Medicine, Nova Southeastern University
MEMBERSHIPS: American College of Cardiology, Society of Cardiac Angiography Intervention, American Heart Association, Collier County Medical Society, European Society of Cardiology









