By Amy Hoffmann Schenk, RN, BSN, MS Ed, Community Engagement Lead Neuropsychiatric Research Center of SW Florida
 “Why is my wife so mean to me?” “My grandfather got downright ornery, wouldn’t do anything we asked, and he yells all the time.” “My mother is always so nervous and fidgety. When I tell her to relax, she says unkind things to me.”
“Why is my wife so mean to me?” “My grandfather got downright ornery, wouldn’t do anything we asked, and he yells all the time.” “My mother is always so nervous and fidgety. When I tell her to relax, she says unkind things to me.”
Are any of these situations familiar? For individuals living with Alzheimer’s disease or another dementia, sometimes it may seem like your loved one is being difficult. As a caregiver, this can be very frustrating. One of the best phrases to remember goes like this: a person with dementia is not giving you a hard time they are having a hard time. What does that mean exactly?
Alzheimer’s disease is a brain disease that impacts everything the brain controls. Memory, speech, logical thinking, reasoning, executive functioning, and expressions, are just some of the things that can be impacted. And while it may seem that someone is behaving in a hateful, ornery, or unkind manner, it can be helpful to realize that what is being seen and experienced is likely a result of the impact of the disease on the person. Some of the behavioral expressions may be a result of an underlying unmet need.
According to the Alzheimer’s Association, the individual with the disease is experiencing a biologically profound loss of their ability to negotiate new information and stimulus. This is due to disease, versus their personality. This can be difficult to understand for those who do not have the cognitive impact of this disease. To make things more challenging, sometimes the behavior observed is different from day to day, even hour to hour.
It is estimated that between 30 to 50% of individuals with Alzheimer’s disease experience agitation and irritability at some time during the course of their illness. What we may see is restlessness, nervousness, short temperedness, expressions of frustration and lack of cooperation. Some individuals may pace, some may perform repetitive motions, others may be quicker to argue and raise their voice and may appear to be in total denial of the facts we present to them.
What looks like denial in someone with the disease may be related to the changes in the brain which impact cognition and awareness. As a result, approaches to address our observations and concerns may not be effective or achieve the response desired. Having a factual, logic based response many times is not effective.
What approaches and techniques can work? Unfortunately, it is true that responses that can be effective with one person may not work with another. As many caregivers know, the same approach used with the same individual may have a different response on a day to day and even on an hour to hour basis. Having some general considerations can be helpful. Here’s an acronym to help: CARE
C: Consistently Calm: That may seem impossible some days, and that is to be expected. Doing your best to respond to what you are seeing in a calm, nonjudgmental and caring manner can help.
A: Appropriate Activities: Many times, when individuals are bored or don’t have structure, some challenging behavioral expressions may present themselves. Many things can be considered an activity and it’s important that the chosen activity is appropriate for the individual and tailored to their interests as much as possible.
Another important consideration is time of day, length of activity and inviting someone to participate versus insisting on participation. A saying that can reflect interacting with someone with Alzheimer’s disease is “the more you insist, the more they will resist.” None of us like to be told what to do and being invited or asked to do something, versus being told may be more successful.
R: Regular Routine: Keeping a consistent routine, based on your loved one’s habits can help decrease anxiety and preserve independence. The Alzheimer’s Association suggests considering the person’s likes, dislikes, strengths, and abilities when developing the routine. Knowing the times of day that the person functions best and allowing ample time for activities is essential. While a consistent schedule is helpful, building in flexibility and going with the flow is also an important consideration.
E: Engagement and Empathy: Include the person in everyday activities and let them help, even if they don’t do things exactly the way you hope they would. Include them in things they enjoy. Participating in your faith community, helping in the garden, running errands, having a meal are all ways to engage. Being empathetic and understanding are also tools that can be valuable. It can be challenging to be a caregiver, and recognizing that it must also be difficult for the person with the disease as well provides perspective.
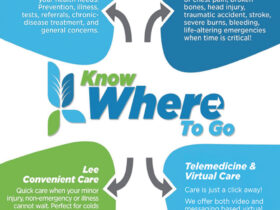
Have you noticed subtle changes in your loved one’s memory? It’s not uncommon for memory lapses to occur as we age, but when they start impacting daily life, it’s essential to take action.
Connect with the experienced team at the Neuropsychiatric Research Center at 239-939-7777, where we have a proven track record of helping individuals and families navigate memory related challenges. Remember, you’re not alone on this journey. #MemoriesMatter
Neuropsychiatric Research Center
239-939-7777 | nprc-swfl.com
14271 Metropolis Avenue., Fort Myers, FL
References:
Anxiety & Agitation | Alzheimer’s Association
https://www.alz.org/help-support/caregiving/stages-behaviors/
anxiety-agitation
Agitation and Dementia: Prevention and Treatment Strategies in Acute and Chronic Conditions – PMC (nih.gov)