By Susan Keller, BSN, MPH
 On election day, 2022, I enthusiastically rode my bicycle to the local voting precinct to cast my vote. After quicky stopping bicycle, my foot failed to clear the bicycle seat, sending me crashing onto my left hip.
On election day, 2022, I enthusiastically rode my bicycle to the local voting precinct to cast my vote. After quicky stopping bicycle, my foot failed to clear the bicycle seat, sending me crashing onto my left hip.
I lay in the street motionless, in childbirth like pain, unable to properly move my left leg.
I didn’t wait for someone to ask if they should call an ambulance, I begged bystanders to call an ambulance, I asked every minute, where was the ambulance? Two guys lifted me up. The pain and abnormal position of my dangling leg was a sure indication something was wrong.
The ambulance ride to the hospital seemed to take hours, yet ER triage time seemed to take just minutes. There was a flurry of healthcare team introductions, forms to sign and then preparation for an x-ray.
My belt wasn’t even unbuckled when the nurses knew my new pair of J Crew shorts would have to be cut off. I was in significant pain and didn’t care.
I was fortunate to have fallen mid-day, as the hospital had an orthopedic surgeon on call and readily accessible.
Dr. Robert Swift, my orthopedic surgeon addressed the fracture head on, preparing me for surgery, which I surely thought could wait at least three days. He informed me this was not the case, as the situation was an urgency.
Two hours later, my sedation had worn off and I was welcomed to the orthopedic unit. I thought surely an indwelling catheter would have been inserted so I wouldn’t have to get out of bed to pee, but there was none. Getting out of bed, if to just go to the bathroom, was instrumental in the recovery process.
My mindset changed from “I can’t move” to how to “how can I move so it’s not painful”?
During my week stay at the hospital, the nursing staff inspected the surgical dressing, assessed my pain and recovery progress. Physical therapy taught me how to reposition myself, get me out of bed and how to walk using a walker.
The goal of the healthcare team was to ensure I was healing and to provide me with the knowledge, motivation and tools to have a successful recovery at home. I was transferred to an inpatient rehabilitation program at a local rehabilitation hospital. Physical therapy was scheduled daily, progressing from two sessions a day, increasing to four times a day by week’s end.
Home physical therapy was scheduled before the hospital discharge. Physical therapy reinforced the leg exercises taught in the hospital. I progressed from using a walker to using a rollator. While I was sometimes uncomfortable performing the exercises, they were instrumental in my healing process. Ice, pain medication and my mantra “I can do this” helped the healing process even more.
The partnership between my health care provider and orthopedic surgeon gave me peace of mind that progress was being made.
Almost two months after my hip surgery successfully completing physical therapy. I rode my bike past my neighbors, only to find her sprawled in her driveway, in obvious pain. We elected to drive to the hospital. While she was fortunate not to need surgery, the CT scan revealed she had a pelvic fracture. Fortunately, Dr. Swift was her orthopedic surgeon as well.
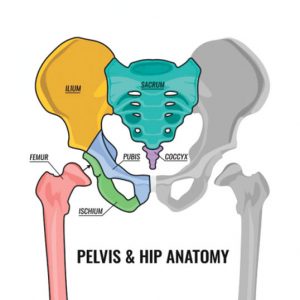
There is confusion about what exactly a hip fracture is. Is it a femur fracture? Is there a hip bone? Is a pelvic fracture worse? The hip is made up of the femur and the pelvis. When there is a fall onto the side all of those structures are at risk. There can be fractures of the femur through the top part of the bone. There can be fractures that separate the ball of the femur through the neck. There can be surrounding fractures around the pelvis on the front and even into the back of the pelvis. Many of these fractures are referred to as “hip fractures.”
Osteoporosis is a disease in which the bone’s mineral density and mass is decreased, thereby negatively impacting bones strength, thereby increasing the risk of bone fracture (broken bones).
Risk factors for osteoporosis include:
• Race
• Women greater then.
• Age (age 50 and over)
• Men with low testosterone levels
• Smokers and heavy drinking (more than two drinks
a day on most days)
• Weight (less than 125 pounds)
• Previous bariatric surgery
• Previous fragility fracture as a senior
• Kidney failure, inflammatory bowel disease, rheumatoid arthritis, liver disease or an eating disorder
• Taking oral corticosteroids on a daily basis, or other high-risk medications (e.g., thyroid hormone replacement, immunosuppressant drugs, warfarin)
Osteopenia is a loss of bone mineral density (BMD) that weakens bones, normally this occurs first and if untreated can progress to Osteoporosis.
Signs and risk factors, including:
• Height loss
• Receding gums
• Curved, stooped forward shape of the spine
• Lower back pain
• Prior fragility fractures with mild impact can occur
at the shoulder, elbow, wrist, spine and ankle.
My hip fracture motivated me to reduce my osteoporosis risk factors that I could control, including maintaining a proper weight, working on flexibility and range of motion exercise, performing resistance exercises, eating a healthy diet, and participating in daily weight bearing activities.
A fall is just not a fall, see your Orthopedic Surgeon or go to the ER. In my case Dr. Swift worked to get me to the operating room urgently. This prevented me from lying in a hospital bed in pain waiting to go to the Operating room. Early intervention got me out of bed and on to a speedy recovery. Early intervention was a key to my early recovery, and a hallmark of Dr. Swift’s commitment to care.
Feel free to contact Dr. Robert Swift or ask for him in the Emergency Department if you fall and have concern for a fracture.
Blue Sky Orthopedic
730 Goodlette-Frank Rd. N., Ste 205,
Naples, FL 34102
(239) 877-4662 | www.drrobertswift.com