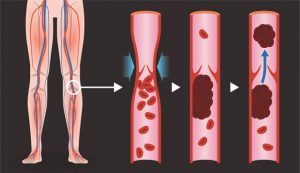
 Deep vein thrombosis (DVT) occurs when a blood clot (thrombus) forms in one or more of the deep veins in the body, usually in the legs. Deep vein thrombosis can cause leg pain or swelling. Sometimes there are no noticeable symptoms.
Deep vein thrombosis (DVT) occurs when a blood clot (thrombus) forms in one or more of the deep veins in the body, usually in the legs. Deep vein thrombosis can cause leg pain or swelling. Sometimes there are no noticeable symptoms.
You can get DVT if you have certain medical conditions that affect how the blood clots. A blood clot in the legs can also develop if you don’t move for a long time. For example, you might not move a lot when traveling a long distance or when you’re on bed rest due to surgery, an illness, or an accident.
Deep vein thrombosis can be serious because blood clots in the veins can break loose. The clots can then travel through the bloodstream and get stuck in the lungs, blocking blood flow (pulmonary embolism). When DVT and pulmonary embolism occur together, it’s called venous thromboembolism (VTE).
Symptoms of DVT and PE
Deep vein thrombosis (DVT) symptoms can include:
• Leg swelling
• Leg pain, cramping, or soreness that often starts in the calf
• Change in skin color on the leg — such as red or purple, depending on the color of your skin
• A feeling of warmth on the affected leg
The warning signs and symptoms of a pulmonary embolism include:
• Sudden shortness of breath
• Chest pain or discomfort that worsens when you take a deep breath or when you cough
• Feeling lightheaded or dizzy
• Fainting
• Rapid pulse
• Rapid breathing
• Coughing up blood
Risk Factors of DVT and PE
Many things can increase the risk of developing deep vein thrombosis (DVT). The more risk factors you have, the greater your risk of DVT. Risk factors for DVT include:
• Age. Being older than 60 increases the risk of DVT. But DVT can occur at any age.
• Lack of movement. When the legs don’t move for a long time, the calf muscles don’t squeeze (contract). Muscle contractions help blood flow. Sitting for a long time, such as when driving or flying, increases the risk of DVT. So does long-term bed rest, which may result from a lengthy hospital stay or a medical condition such as paralysis.
• Injury or surgery. Injury to the veins or surgery can increase the risk of blood clots.
• Pregnancy. Pregnancy increases the pressure in the veins in the pelvis and legs. The risk of blood clots from pregnancy can continue for up to six weeks after a baby is born. People with an inherited clotting disorder are especially at risk.
• Birth control pills (oral contraceptives) or hormone replacement therapy. Both can increase the blood’s ability to clot.
• Being overweight or obese. Being overweight increases the pressure in the veins in the pelvis and legs.
• Smoking. Smoking affects how blood flows and clots, which can increase the risk of DVT.
• Cancer. Some cancers increase substances in the blood that cause the blood to clot. Some types of cancer treatment also increase the risk of blood clots.
• Heart failure. Heart failure increases the risk of DVT and pulmonary embolism. Because the heart and lungs don’t work well in people with heart failure, the symptoms caused by even a small pulmonary embolism are more noticeable.
• Inflammatory bowel disease. Crohn’s disease or ulcerative colitis increases the risk of DVT.
• A personal or family history of DVT or PE. If you or someone in your family has had one or both conditions, you might be at greater risk of developing DVT.
• Genetics. Some people have DNA changes that cause the blood to clot more easily. One example is factor V Leiden. This inherited disorder changes one of the clotting factors in the blood. An inherited disorder on its own might not cause blood clots unless combined with other risk factors.
Prevent Blood Clots
Traveling often includes sitting for periods, which can increase your chances of developing a deep vein thrombosis (DVT), a type of blood clot that forms in a large vein. Part of the clot can break off and travel to the lungs, causing a sudden blockage of arteries in the lung, known as a pulmonary embolism. Though these types of blot clots are rare, they are very serious and can cause death. Find out what steps you can take to prevent blood clots during travel.
The Vascular and Vein Center at Gulfcoast Surgeons is one of the first and most respected vein clinics in Southwest Florida. Our surgeons, Dr. Abraham Sadighi and Dr. Johan Escribano have performed thousands of vascular and vein surgeries over the past 28 years. We focus on diseases of the vascular system that can range from harmless but unattractive spider veins to dangerous conditions such as peripheral artery disease. Our caring and dedicated team will help you identify problems and offer the best treatment options for you at any of our three locations.
Call the Vascular & Vein Center at Gulfcoast Surgeons today at (239) 344-7061 to make an appointment with a vascular surgeon who specializes in arteries and veins.
Vascular & Vein Center at Gulfcoast Surgeons
877-LEG-PAIN
gulfcoastsurgeons.com
Fort Myers
8010 Summerlin Lakes Dr., Ste. 100
Fort Myers, FL 33907
Cape Coral
1003 Del Prado Blvd., Ste. 303
Cape Coral, FL 33990
Bonita Springs
24301 Walden Center Dr., Ste. 102
Bonita Springs, FL 34134










