By Joseph Magnant, MD, FACS, RPVI and Jill Layman, MSN, FNP-BC
With authorities proclaiming our present state to be the “new normal,” we must assess what that means. Many people have had to transition to self-isolation as they work from home and have limited contact with the public. While this isolation is essential for decreasing the spread of COVID-19, it can result in a more sedentary lifestyle that limits the opportunity for healthy activities and may lead to increased weight gain. For people with venous disease, sitting or standing for prolonged periods of time may lead to weight gain and result in significant pain and discomfort due to venous disease.
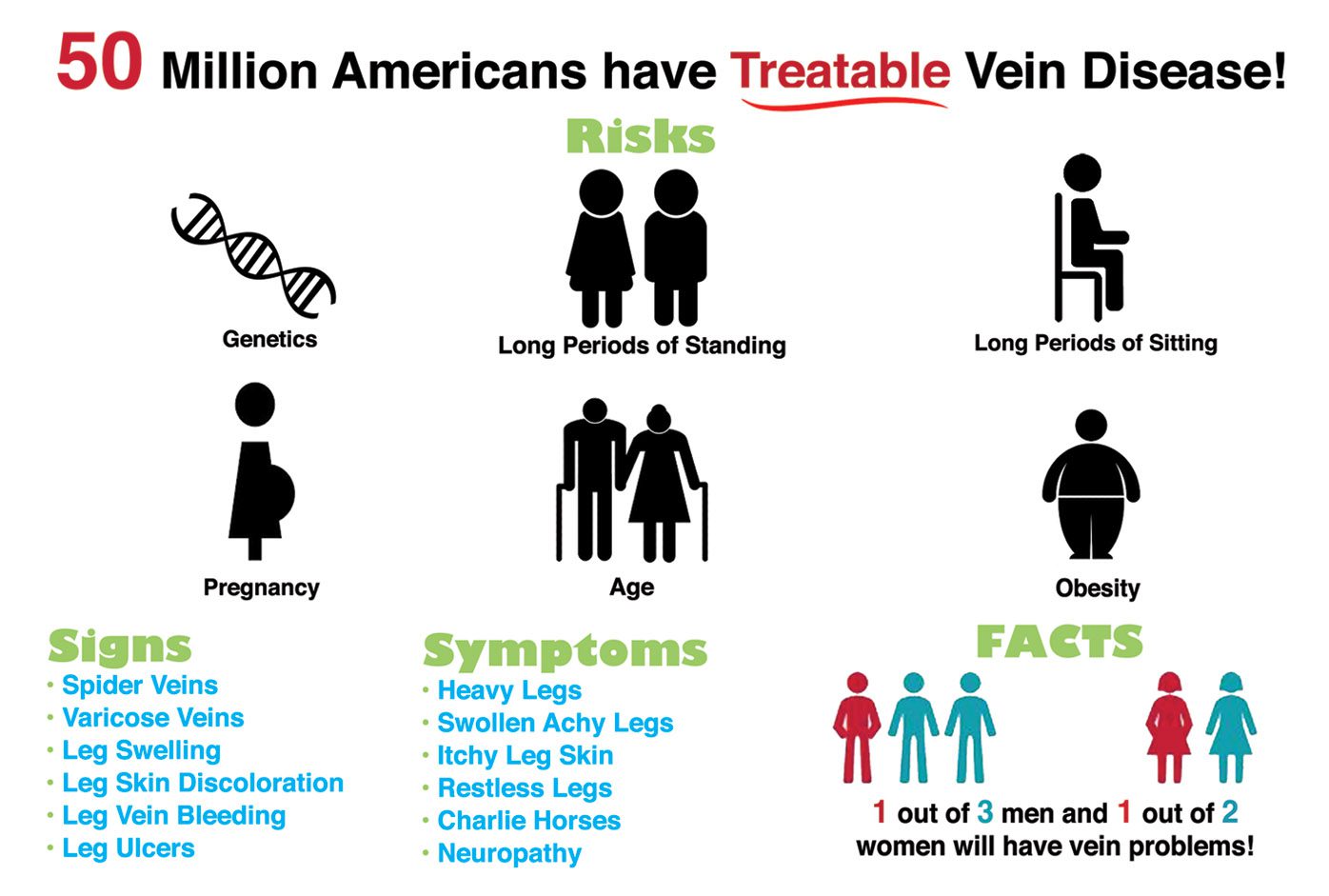
Veins are blood vessels that are specially designed to pump blood toward the heart against the force of gravity. Inside the veins, there are a series of one way or check valves that open and close with the rhythm of muscle contractions. Healthy valves close tightly, keeping blood moving upward toward the heart. With vein disease, or venous insufficiency, the valves do not properly close. This allows blood to flow back down the legs and pool in the veins. The pooled blood can lead to bothersome symptoms, such as swollen, achy legs and leg cramping, most commonly worse by the end of the day. More severe venous disease cases may manifest or present as varicose veins and skin changes that may process to bleeding veins and leg ulcers.
Venous insufficiency is a very common and underdiagnosed condition affecting millions of Americans. Heredity is a major risk factor and the disease becomes more prevalent in both men and women after age 50. Other risk factors include a history of blood clots or DVT, obesity, standing or sedentary occupation, and female gender and prior pregnancies.
Times of stress and change can disrupt healthy behaviors. It’s possible to take charge and make healthy habits at home by continuing to eat nutritious foods and engaging in physical activity. Furthermore, certain habits will help lessen the symptoms associated with venous disease.
• Regular exercise
– Walking or biking for 30 minutes per day, 5-7 days per week will help reduce aching, pain, or tiredness in your legs
• Elevate your legs
– Elevating your legs above your heart for ten minutes once or twice daily may diminish aching and swelling
• Maintain a proper weight
– Even moderate weight loss may reduce aching in the legs due to varicose veins
• Wear compression hose
– Its best to wear compression hose that are labeled as “graduated,” as this benefits vein function the most
• Move your legs frequently
– Flexing your ankles ten times will pump the blood out of your veins like walking does. Repeat this every ten minutes when standing or sitting. Also, try to walk at least two minutes every half hour.
Navigating this “new normal” may seem daunting at times, but it’s important to be proactive in your personal health by keeping your lifestyle active even when at home.
Patient Case Study: For example, take C.D., a 58 year old female who presented through a podiatrist for a evaluation of venous insufficiency. She had been told by several physicians that she had “fat and swollen legs”, and since she did not have any visible bulging varicose veins, venous insufficiency was never considered as a potential cause.
Clinically, her legs were swollen, red, tender and extremely tight to the point that she could not perform activities of daily living. She decided to search further for a curable cause and her podiatrist astutely referred her for a venous evaluation. Her ultrasound subsequently confirmed severe superficial venous insufficiency. Endovenous closures
were performed on both legs, 2 weeks apart and she returned for her post-op follow-up, smiling from ear to ear, with ankle bones that she could actually see for the first time in many months. The swelling had resolved, and she remarked that she was wearing tennis shoes, rather than slippers, for the first time in nine months.
Whether you are recently retired or heading off to college, if you are concerned about your lower extremity symptoms of fatigue and achiness, or if you have obvious signs of venous disease such as varicose veins, swelling or skin discoloration, please consider a venous evaluation. Remember, you do not have to have visible signs to have venous disease.
For more information please visit our website at WeKnowVeins.com or contact our office at 239-694-VEIN (8346).
Joseph G. Magnant,
MD, FACS, RPVI
Board Certified Vascular Surgeon
SWFL’s first IAC Accredited Vein Centers (Fort Myers & Bonita Springs)
1500 Royal Palm Square Blvd., Suite 104, Fort Myers, Florida | 3359 Woods Edge Circle, Suite 102, Bonita Springs, Florida









