By Dr. Aneley Yegezu Hundae, M.D., FACC
 Peripheral vascular disease (PVD) is a condition that affects the blood vessels outside the heart and brain, commonly referring to issues in the arteries and veins of the extremities. This condition can significantly impact an individual’s quality of life, potentially leading to pain, limited mobility, and even serious complications. In this article, we delve into the causes, symptoms, diagnosis, and treatment options for peripheral vascular disease.
Peripheral vascular disease (PVD) is a condition that affects the blood vessels outside the heart and brain, commonly referring to issues in the arteries and veins of the extremities. This condition can significantly impact an individual’s quality of life, potentially leading to pain, limited mobility, and even serious complications. In this article, we delve into the causes, symptoms, diagnosis, and treatment options for peripheral vascular disease.
Causes of Peripheral Vascular Disease
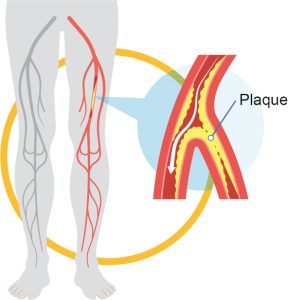
PVD is often attributed to atherosclerosis, a condition where fatty deposits build up in the arteries, causing them to narrow and reduce blood flow. This reduced blood flow can lead to pain and other symptoms. Risk factors for PVD include smoking, diabetes, high blood pressure, high cholesterol, obesity, and a family history of cardiovascular diseases.
Symptoms and Progression
The symptoms of PVD can vary depending on the severity and location of the affected blood vessels. Common symptoms include cramping, pain, or fatigue in the legs or arms during physical activity, known as intermittent claudication. As the condition worsens, pain may also occur during rest. Other signs include numbness, tingling, slow-healing wounds, and changes in skin color or temperature. If left untreated, PVD can lead to complications such as non-healing ulcers and even gangrene.
Diagnosis and Evaluation
A medical professional will diagnose PVD through a combination of patient history, physical examination, and diagnostic tests. Ankle-brachial index (ABI) is a common test that compares blood pressure in the ankle with that in the arm to determine blood flow. Doppler ultrasound, angiography, and magnetic resonance angiography (MRA) are also used to assess blood vessel condition and location of blockages.
Treatment Options
1. Lifestyle Changes: Adopting a healthy lifestyle is crucial. Quitting smoking, managing diabetes, maintaining a healthy weight, and engaging in regular exercise can improve blood flow and alleviate symptoms.
2. Medications: Medications to manage PVD may include antiplatelet drugs to prevent blood clots, cholesterol-lowering medications, and medications to control blood pressure and improve circulation.
3. Angioplasty and Stenting: In cases of severe blockages, angioplasty may be performed. This involves inserting a catheter with a deflated balloon into the blocked vessel and inflating it to widen the artery. A stent may also be placed to keep the artery open.
4. Surgery: Bypass surgery involves creating a new path for blood flow by grafting a healthy blood vessel to bypass the blocked area. This is typically considered when other treatments are not effective.
5. Laser and Atherectomy: These minimally invasive procedures involve using laser or rotating blades to remove plaque from artery walls.
6. Exercise Programs: Supervised exercise programs help improve circulation and reduce symptoms in individuals with PVD. These programs combine aerobic and strength exercises.
Preventive Measures
While PVD is a serious condition, certain measures can reduce the risk of developing it. Regular health check-ups, managing underlying health conditions, eating a balanced diet, staying physically active, and avoiding tobacco are all crucial for maintaining vascular health.
Peripheral vascular disease is a complex condition that can significantly impact an individual’s well-being and functionality. Recognizing the risk factors, understanding the symptoms, and seeking timely medical attention are vital steps toward managing the disease effectively. By adopting a healthy lifestyle and following recommended treatments, individuals can improve their vascular health and enhance their overall quality of life. If you suspect you may have symptoms of PVD, consult a medical professional for proper diagnosis and guidance.
Dr. Aneley Yegezu Hundae, M.D., FACC
invasive cardiology and advanced heart failure management
Dr. Hundae received his Premedical and Doctor of Medicine Degree from Jimma University School of Medicine. He completed his Internal medicine Residency at Mercer University School of Medicine. His Heart Failure/Heart Transplant fellowship at the University of Miami Cardiovascular Fellowship Program. Cardiovascular fellowship at Baylor University Medical Center.
Board certifications
• Cardiology
• Advanced Heart Failure and Transplant
• Nuclear Cardiology
• Comprehensive Echocardiography
• Internal Medicine
3161 Harbor Blvd, Suite A, Port Charlotte, FL 33952
(941) 235-8892
www.portcharlottecardiology.com








