Written by Regenexx Tampa Bay, Regenerative Medicine
 Oftentimes, patients ask us what they can do to improve their joint cartilage and prevent arthritis. Cartilage acts as a cushion between the bones to protect our joints by absorbing shock.
Oftentimes, patients ask us what they can do to improve their joint cartilage and prevent arthritis. Cartilage acts as a cushion between the bones to protect our joints by absorbing shock.
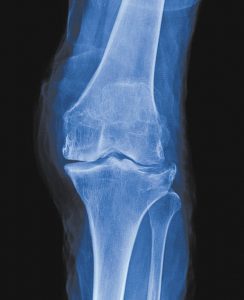
The visual evidence of arthritis seen on imaging studies can be due to the decrease in quantity and quality of the cartilage, the decrease in joint space width, the formation of bone spurs, and degenerative changes in the bone underlying the cartilage. Besides wear and tear, there is also a biologic/internal component that affects cartilage.
The Truth About Cartilage Loss
Cartilage, in of itself, does not have nerve endings. Therefore, cartilage loss is NOT a direct source of pain. It is, however, the visual evidence that arthritis exists. That is, there are destructive substances in the joint that are breaking down the tissue. The cartilage is the victim of the arthritic disease.
You might be surprised to learn that people can have virtually no cartilage in a part of a joint (“bone on bone”) and have no pain at all. This is actually very common. On the other hand, a person can have robust amounts of cartilage and have a tremendous amount of pain – again, this is very common as well. The point is that cartilage loss is a sign of arthritis and protecting your cartilage is a way of limiting the effects of the arthritic process.
What Causes Joint Pain?
There are a number of structures that do cause pain. The synovial lining of the joint is rich in nerve endings that sense pain and is responsible for producing healthy fluid and lubricating substances. With arthritis, the synovial lining can become bumpy and painful. It will also produce abnormal inflammatory fluid that breaks down tissue in the joint. Determining what’s in that fluid and how to control the synovial lining is one of the keys to halting arthritis.
Another source of pain in a joint is the bone underneath the cartilage. This bone is quite hardy and able to tolerate heavy loads often without any problems even when there isn’t any cartilage to protect it. There are times when the bone in areas of decreased cartilage begins to breakdown and become swollen representing little micro-breaks in the bone. These bone marrow lesions can sometimes be painful and can only be seen on an MRI.
Can We Re-grow Cartilage?
Getting cartilage to re-grow is an admirable goal and it may one day be possible to consistently do this, but it seems that it’s actually more important to keep the synovial lining under control and to strengthen the bone under the cartilage so that it can withstand more pressure. It is also important to make sure that there is stability around the joint – that is, the ligaments, tendons, muscles, and nerves are healthy and functioning normally.
Stem cells can help cartilage to regrow but it is inconsistent and minimal at this time (despite what you may have heard). They can, however, improve the quality of the remaining cartilage, the strength of the bone, reprogram the synovial lining so that it produces healthy protective chemicals instead of destructive ones, and strengthen the ligaments and tendons so that there is better stability around the joint. Using stem cells in this way requires working with a highly trained physician who performs the proper analysis and executes a procedure to precisely inject the tissues that are in need of improvement.
Receiving a stem cell injection blindly into a joint by someone who dabbles in this approach is not the way to go.
The key to understanding how to keep more cartilage as you age is to understand what causes cartilage loss. Here are the most common causes of cartilage loss along with a few solutions to help prevent it.
1. Obesity (Mechanical)
Physics has taught us that being heavier places more wear-and-tear forces on our cartilage and therefore, arthritis.
Although it can be tough to accomplish, losing weight is the ultimate solution to improve symptoms and slow the progression of arthritis.
2. Obesity (Biochemical)
Not only does obesity break down cartilage by wear and tear, but is also can cause changes in the patient’s insulin-response system that can break down cartilage. This is referred to as “metabolic syndrome.”
We recommend reducing carbohydrate and sugar intake to minimize spikes in blood sugar and insulin release.
3. Trauma
A sudden traumatic event, such as a sports injury, can injure the cartilage surface and potentially cause a weak spot in the cartilage. If weak spots are present, cartilage can break down faster with normal forces.
Before the issue becomes bigger, look for regenerative medicine cell-based solutions for cartilage repair, such as platelet-rich plasma (PRP) or stem cell injections.
4. Joint Instability
Injured ligaments can cause joints to move around too much and cause joint instability. All of this extra unnatural motion can slowly continue to injure the cartilage in the joint, eventually leading to arthritis.
Injections like prolotherapy, PRP, and stem cells in our clinical experience can help reduce instability whether the ligament is loose or torn (partial or nonretracted). In more severe cases, surgery may be needed.
5. Poor Nutrition
Poor dietary habits and lack of proper nutrition can cause major issues with not only your cartilage and your musculoskeletal system but your entire body. What you eat can turn on or off the genes in your body that protect your cartilage.
It is essential to know what is and what is not good for you and your body. Consider introducing supplements like Glucosamine and chondroitin into your diet to enhance cartilage health.
6. Medications
Surprisingly, the most common medications that are injected into arthritic joints for relief such as local anesthetics and steroids are also likely the most toxic to cartilage. Commonly used NSAID medications, like ibuprofen, naproxen, and celecoxib have also been shown to have negative effects on cartilage cells.
We recommend staying away from “cortisone shots,” NSAIDS, and other drugs when not essential.
7. Lack of Exercise
Besides leading to many other health issues, lack of exercise can create problems with our joints. Joints are made for movement. Regular exercise along with utilizing the proper techniques for those exercises is essential.
If you have cartilage loss, you may want to switch from high-impact exercises to low-impact activities to protect your existing cartilage. If you have normal, healthy joints, keep running and exercising regularly, it is likely protective.
8. Poor Alignment and Biomechanics
If you have asymmetrical cartilage loss (loss of cartilage in one knee and not the other), you may have a body-alignment problem that is wearing down certain joints faster than others.
Working with a skilled physical therapist can help you get your muscles balanced and fine-tune your body so that it is biomechanically optimized.
9. Aging and Genetics
Unfortunately, older patients seem to have less cartilage and some people simply have the genetic makeup for weaker cartilage.
While there isn’t much that we can do about our genes, we can influence the ways our genes are expressed by leading a healthier lifestyle overall.
Understanding why cartilage breaks down, adhering to a healthy lifestyle, and utilizing regenerative options like PRP and stem cells seems to be the best strategy for maintaining healthy cartilage and decreasing the pain associated with arthritis.
Regenexx Tampa Bay
RegenTampaBay.com
8600 Hidden River Parkway, Suite 700
Tampa, FL 33637
941-254-2757
Dr. James Leiber
James Leiber, DO, is the founder and medical director of Regenexx Tampa Bay. He is a former officer, physician, and educator in the Air Force, including personal physician to the vice president and president at the White House. He is triple board certified in Neuromusculoskeletal Medicine (AOBNMM), Pain Medicine (CAQPM), and Family Medicine (ABFM), as well registered in Musculoskeletal Sonography (RMSK).
Dr. Leiber specializes in Interventional Regenerative Orthopedics with years of experience and is honored to have been the first Regenexx Network Provider in Florida. In 2012, Dr. Leiber began offering the nation’s most advanced non-surgical stem cell and platelet treatments (PRP) for injuries and arthritis under image guidance utilizing ultrasound and fluoroscopy (X-ray).
He is a published author, presenter, and is currently the program director for the Interventional Orthopedic Foundation.
He lives in Sarasota, Florida with his wife and teenage daughter. Dr Leiber travels regularly to Denver, to teach regenerative orthopedic techniques to fellow doctors, and to Grand Cayman, where he is also licensed to treat patients.
Ron Torrance II, D.O. – Board Certified in Sports Medicine and recent co-author of Exercise 2.0 for Regenexx and author of the 2018 best paper of the year on The Concussed Athlete. Dr. Torrance has achieved semi-professional ranking as a beach volleyball player and trains as a competitive CrossFit athlete.
Ignatios Papas, D.O. – Specializes in Physical Medicine and Rehabilitation. He is a research collaborator with Columbia and Cornell University on multiple projects. Dr. Papas enjoys spending time with his wife and son, playing soccer, practicing guitar, and listening to historical podcasts.
Michael Amoroso, M.D. is Board Certified by the American Board of Anesthesiology and the American Board of Pain Medicine. He has been a long-time runner and brings a vast amount of experience to his role at Regenexx Tampa Bay. Dr. Amoroso travels frequently back to his home in New Jersey to visit his children and small grandchildren.









