By Russell Becker, DO
 Living with diabetes requires vigilant attention to many aspects of health, but one of the most serious complications involves the feet. At Vascular Center of Naples, we understand that peripheral arterial disease (PAD) combined with diabetes creates a dangerous situation that can lead to diabetic foot ulcers—wounds that refuse to heal and can threaten limb preservation if left untreated.
Living with diabetes requires vigilant attention to many aspects of health, but one of the most serious complications involves the feet. At Vascular Center of Naples, we understand that peripheral arterial disease (PAD) combined with diabetes creates a dangerous situation that can lead to diabetic foot ulcers—wounds that refuse to heal and can threaten limb preservation if left untreated.
Understanding Peripheral Arterial Disease
Peripheral arterial disease occurs when plaque builds up in the arteries that carry blood to your limbs, particularly the legs and feet. This buildup narrows the arteries, reducing blood flow to these extremities. For individuals with diabetes, PAD is especially common and particularly problematic. High blood sugar levels accelerate the development of arterial plaque, making diabetic patients up to four times more likely to develop PAD than non-diabetics.
The reduced blood flow from PAD means that tissues in the feet and legs receive less oxygen and fewer nutrients. This compromised circulation makes it extremely difficult for any wounds or injuries to heal properly, setting the stage for serious complications. Many patients don’t realize they have PAD until a minor injury fails to heal, highlighting the importance of regular vascular screenings for anyone living with diabetes.
The Diabetic Foot Ulcer Crisis
Diabetic foot ulcers are open sores or wounds that develop on the feet of people with diabetes. These ulcers typically form on pressure points such as the bottom of the foot or on areas subjected to friction. What makes them particularly dangerous is the combination of three factors: poor circulation from PAD, nerve damage (neuropathy) that prevents people from feeling pain or injury, and the body’s impaired healing response due to diabetes.
When PAD is present alongside diabetes, even a minor blister, cut, or callus can evolve into a serious ulcer. Without adequate blood flow, the body cannot deliver the white blood cells and nutrients necessary to fight infection and repair tissue. The ulcer may deepen, become infected, and in severe cases, lead to gangrene—tissue death that can necessitate amputation.
Statistics paint a sobering picture: approximately fifteen percent of people with diabetes will develop a foot ulcer during their lifetime, and those with PAD face significantly higher risks. Even more concerning, diabetic foot complications account for more hospitalizations than any other diabetic complication, and they remain a leading cause of non-traumatic lower limb amputations in the United States.
Warning Signs to Watch
At Vascular Center of Naples, we emphasize the importance of recognizing early warning signs. PAD symptoms include leg pain or cramping when walking that improves with rest, coldness in the lower leg or foot, slow-growing toenails, shiny skin on the legs, and wounds on the feet or legs that heal slowly or not at all. Any change in skin color, development of sores, or unusual sensations should prompt immediate medical attention.
For diabetic foot ulcers specifically, watch for drainage on your socks, unusual swelling, redness, or warmth around a wound, and any opening on the foot regardless of size. The absence of pain doesn’t mean absence of danger—neuropathy can mask serious problems. Some patients discover ulcers only during routine foot checks, underscoring why daily self-examinations are so crucial.
Prevention and Treatment
Prevention remains the most effective strategy. Daily foot inspections, proper footwear, controlled blood sugar levels, and regular vascular screenings can prevent many complications. Professional foot care, including regular examinations by healthcare providers experienced in diabetic foot care, is essential. Never walk barefoot, even indoors, and always check shoes for foreign objects before wearing them.
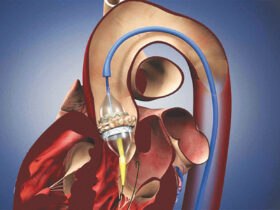
When PAD is detected, treatment options range from lifestyle modifications and medications to advanced interventions. These may include angioplasty to open blocked arteries, stent placement to keep vessels open, or bypass surgery for severe cases. Restoring adequate blood flow is crucial for healing existing ulcers and preventing new ones.
For established diabetic foot ulcers, treatment requires a comprehensive approach: pressure offloading through specialized footwear or casts, aggressive infection control with appropriate antibiotics, meticulous wound care with advanced dressings, and most importantly, addressing the underlying vascular disease. Our team at Vascular Center of Naples specializes in advanced vascular interventions that restore blood flow, giving ulcers the best chance to heal and helping patients avoid amputation.
Take Action Today
If you have diabetes, don’t wait for problems to develop. Regular vascular screenings can detect PAD before it leads to serious complications. At Vascular Center of Naples, we’re committed to preserving limb health through early detection, expert treatment, and compassionate care. Your feet carry you through life—let us help you protect them.
Call us today at 239-431-5884.
1875 Veterans Park Dr. Suite 2203
Naples, FL 34109
239-431-5884
www.VascularCenterNaples.com