Written by Dr. Paul M. Graham
 Platelet rich plasma (PRP) is a new and exciting treatment option for hair loss currently being offered by many dermatologists across the country. Patients that have failed a variety of treatment options for hair loss are now seeing incredible results with PRP therapy. Historically, hair transplants were the only definitive option available for near total hair restoration. The costs of a typical hair transplantation ranges from $3500-$15,000 per session, depending on the experience of the surgeon, the complexity of the problem, and the number of grafts involved. This option is often cost-prohibitive and has prompted the search for new therapies for hair loss, specifically PRP. Taking a more conservative approach, that is using PRP, will give modest results at a fraction of the cost of hair transplantation.
Platelet rich plasma (PRP) is a new and exciting treatment option for hair loss currently being offered by many dermatologists across the country. Patients that have failed a variety of treatment options for hair loss are now seeing incredible results with PRP therapy. Historically, hair transplants were the only definitive option available for near total hair restoration. The costs of a typical hair transplantation ranges from $3500-$15,000 per session, depending on the experience of the surgeon, the complexity of the problem, and the number of grafts involved. This option is often cost-prohibitive and has prompted the search for new therapies for hair loss, specifically PRP. Taking a more conservative approach, that is using PRP, will give modest results at a fraction of the cost of hair transplantation.
Platelet rich plasma (PRP) has been used in the medical community for many years, mainly in the specialties of orthopedic and plastic surgery, as it has shown great effectiveness in the process of wound healing and tissue rejuvenation. PRP has now made its way into dermatology as another treatment option for those suffering from hair loss.
Hair loss can be a very frustrating and extremely challenging problem to treat. It is important to see a dermatologist so that the exact etiology of hair loss can be investigated. A dermatologist will thoroughly evaluate exactly why you are losing hair. Hair loss is often variable and can be caused by a number of different etiologies, some more problematic than others. A detailed history and physical exam will be performed, as well as obtaining the appropriate blood work to evaluate the hair loss. This blog focuses on the use of PRP for male and female pattern hair loss and diffuse hair thinning.
Is PRP an option for you?
If you are a man with male pattern or a woman with female pattern balding, or suffer from diffuse thinning with no identifiable cause, then PRP may be a great option.
What is androgenic alopecia?
Androgenic alopecia, also known as pattern hair loss, is a condition that is often associated with genetic factors and elevated androgenic hormones. This occurs when hormone-susceptible hair follicles shrink in size giving the appearance of hair thinning/loss in a classic and reproducible pattern. Male pattern baldness is the most common type of hair loss and affects 70% of men and 40% of women.
Signs of male and female androgenetic alopecia
1. Gradual onset
2. Increased hair shedding (normal = 100 hairs lost per day)
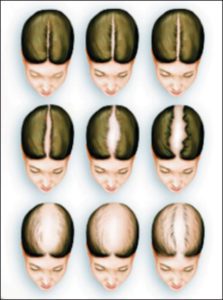
3. Distinct pattern hair loss (as shown above): Men develop a receding hair line and thinning at the vertex scalp; Women develop thinning at the crown and widening of their part
4. Hair goes from being dark, having a large hair shaft diameter, and thick coverage to lighter, smaller hair shafts with thin coverage.
Hair growth occurs in 3 phases: anagen, catagen, and telogen. During the anagen phase, the hair shaft grows in length and diameter over the course of 2-4 years. In catagen phase (2-3 weeks), all growth stops, and the hair shaft slowly loses its connection from the follicle. The telogen phase, otherwise known as the resting phase, last approximately 2-3 months and is characterized by shedding of the hair from the follicle. Androgenic alopecia is both genetic and androgen-dependent, hence its name androgenetic alopecia. Androgens are hormones such as testosterone and dihydrotestosterone (DHT) that when elevated, increase hair shaft miniaturization. Patients with androgenic alopecia also have elevated numbers of telogen hair, leading to increased shedding in the patterns depicted above. Dihydrotestosterone (DHT) is the androgen thought to be directly responsible for this increased shedding that occurs. Testosterone is converted to DHT by the enzyme called 5-alpha-reductase. Patients with a genetic predisposition to develop androgenetic alopecia have increased activity of 5-alpha reductase, increasing the level of circulating DHT.
Minoxidil (Rogaine) is the only FDA-approved topical treatment option for men and women suffering from androgenic alopecia. On the other hand, Finasteride (Propecia or Proscar) is the only FDA-approved oral medication for the treatment of androgenic alopecia in men. Other commonly used treatments include oral contraceptive pills and spironolactone for their anti-androgen effects, hair transplantation, and now PRP.
Propecia works by blocking an enzyme called 5-alpha reductase, therefore decreasing the conversion of testosterone to DHT. It is thought that by decreasing DHT, this will slow the progression of hair follicle miniaturization, leading to retention of pre-existing terminal scalp hairs. Propecia does come with several side effects, which include erectile dysfunction, decreased libido, breast tenderness and gynecomastia (breast enlargement). Be sure to have a detailed discussion with your dermatologist before starting this medication.
Androgenic alopecia is highly associated with numerous genetic factors, but PRP therapy may halt genetically pre-determined hair loss. Deactivated stem cells are present in hair follicles of patients with androgenetic alopecia. PRP contains the growth factors necessary to activate these stem cells, leading to an increase in hair growth. Recent studies support an increase in number of hair follicles and hair density after undergoing PRP treatment, as demonstrated on biopsy specimens 2,3,4.
How does PRP work?
PRP is derived from whole blood. Blood is drawn into a test tube and placed into a centrifuge to separate out the components. Plasma appears as a yellow serum at the top of the test tube, separated from the red blood cells at the bottom. Separating these two components is a layer called the “buffy coat”. The plasma directly above the buffy coat layer is the richest in platelets and immune cells responsible for the beneficial effects of PRP. The remaining plasma is considered platelet poor plasma. PRP contains a high level of both cytokines and growth factors, which function to stimulate inactive stem cells within the hair follicles, promoting increased hair growth.
What are the side effects?
The side effect profile of PRP is relatively mild with only erythema and swelling which last less than 12 hours. PRP is a natural substance derived from the patient’s whole blood, preventing the risk of developing an allergic reaction. Clean or sterile technique is often used to prevent the risk of infection. Although pain is minimized with topical anesthesia, it is not eliminated. Tylenol is often recommended prior to the procedure to limit discomfort.
In summary, there are many options for the treatment and management of hair loss. PRP appears to be a promising therapy for the restoration of male and female androgenic alopecia. Although PRP is relatively new in the field of dermatology, many dermatologists are seeing excellent results with minimal downtime, as compared to more invasive procedures such as hair transplantation. Many etiologies exist that may contribute to hair loss and a thorough evaluation is necessary. Make sure to ask your dermatologist if PRP is right for you!
Associates in Dermatology
To schedule a consultation with Dr. Graham to see if PRP is the right treatment for you, please contact our office at (239) 936-5425. We are located at 8381 Riverwalk Park Blvd, Suite 201, Fort Myers, Florida 33919.
1. Yim, Elizabeth; Nole, Katherine L. Baquerizo; Tosti, Antonella (December 2014). “5α-Reductase inhibitors in androgenetic alopecia.”. Current Opinion in Endocrinology, Diabetes, and Obesity (Review) 21 (6): 493–8.
2. Headington JT, Novak E. Clinical and histological studies of male pattern baldness treated with topical minoxidil. Curr Ther Res Clin Exp. 1984, 36:1098-106.
3. Goldberg, J, Lynne J, Singh B. Autologous platelet-rich plasma for the treatment of pattern hair loss. Amer Jour Clin Derm. 2016. 1-9.
4. Gentile, Peitro. Et al. The effect of platelet rich plasma in hair re-growth: A Randomized Placebo-Controlled Trial. Stems Cells Translational Medicine. 2015;4:1317-1323.
5. Cervelli, V. Et. al. The effect of autologous activated Platelet Rich Plasma (AA-PRP) Injection on Pattern Hair Loss: Clinical and Histomorphometric evaluation. BioMed Research International. 2004; 9 pages.







