By Joe Altepeter, DPM
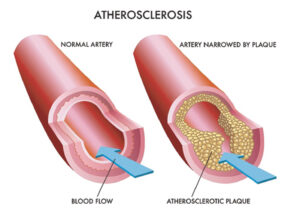 As a podiatrist, I see the silent signs of Peripheral Artery Disease (PAD) every day in my practice. September is PAD Awareness Month, and it’s a critical time to shine a light on this common, yet often misunderstood, circulatory condition. PAD affects millions of people, yet many don’t realize they have it until the disease has progressed to a more serious stage. It’s a condition where plaque builds up in the arteries, narrowing them and reducing blood flow, most commonly in the legs and feet. This poor circulation can lead to significant pain, mobility issues, and, in severe cases, even amputation.
As a podiatrist, I see the silent signs of Peripheral Artery Disease (PAD) every day in my practice. September is PAD Awareness Month, and it’s a critical time to shine a light on this common, yet often misunderstood, circulatory condition. PAD affects millions of people, yet many don’t realize they have it until the disease has progressed to a more serious stage. It’s a condition where plaque builds up in the arteries, narrowing them and reducing blood flow, most commonly in the legs and feet. This poor circulation can lead to significant pain, mobility issues, and, in severe cases, even amputation.
The Role of the Podiatrist
You might wonder why a foot doctor is so concerned with circulatory issues. The answer is simple: the feet are often the first place to show symptoms of PAD. Because the feet are the furthest from the heart, they are the most susceptible to the effects of poor circulation. When I examine a patient’s feet, I’m not just looking at their skin, nails, and bones; I’m also assessing their vascular health. I’m checking for signs like a weak or absent pulse in the feet, non-healing sores, a change in skin color (especially when elevated), and a difference in temperature between the two feet. These are all red flags that can point to PAD.
Many patients come to me with symptoms they attribute to aging or other conditions. They might complain of leg cramps, aching feet, or a feeling of heaviness after walking. These symptoms, known as claudication, are often the classic sign of PAD. It’s a cramp-like pain or fatigue in the leg muscles that occur during exercise and is relieved by rest. It’s the body’s way of telling you that your muscles aren’t getting enough oxygen-rich blood.
Risk Factors and Who’s at Risk
The risk factors for PAD are very similar to those for heart disease and stroke, which is no coincidence—they are all part of a larger systemic problem called atherosclerosis.
The primary risk factors include:
• Smoking: This is the single most significant risk factor. The chemicals in tobacco damage the lining of blood vessels, accelerating the buildup of plaque.
• Diabetes: High blood sugar levels can damage blood vessels throughout the body, making people with diabetes highly susceptible to PAD.
• High Blood Pressure (Hypertension): Uncontrolled high blood pressure puts extra strain on artery walls, leading to damage and plaque formation.
• High Cholesterol: A high level of “bad” cholesterol (LDL) contributes directly to the plaque that clogs arteries.
• Age: The risk of PAD increases with age, particularly after 50.
• Family History: A family history of PAD, heart disease, or stroke also increases your risk.
Why Awareness Matters
Early diagnosis is key to preventing the most severe consequences of PAD. Many people dismiss the early warning signs, thinking it’s just a normal part of getting older. This is a dangerous misconception. If left untreated, PAD can lead to critical limb ischemia, a severe form of PAD that can cause chronic pain, gangrene, and necessitate amputation. In fact, a non-healing foot wound is often the last stop before an amputation, and it’s a situation I work tirelessly to prevent.
Beyond the limb-related complications, PAD is a strong indicator of a higher risk for heart attack and stroke. The same plaque that is clogging your leg arteries is likely present in the arteries supplying your heart and brain. Therefore, a diagnosis of PAD is a wake-up call to manage your overall cardiovascular health more aggressively.
What You Can Do
The good news is that PAD is manageable, and early intervention can significantly improve your quality of life and reduce your risk of serious complications.
• Talk to Your Doctor: If you’re experiencing any symptoms, especially leg pain or cramps, don’t ignore them. Bring it up with your primary care physician or a podiatrist. A simple, non-invasive test called an Ankle-Brachial Index (ABI) can be performed in the office to diagnose PAD. The ABI compares the blood pressure in your ankle to the blood pressure in your arm.
• Lifestyle Changes: Quitting smoking is the most important step you can take. A healthy diet and regular exercise are also essential for managing risk factors like blood pressure, cholesterol, and diabetes.
• Proper Foot Care: As a podiatrist, I can’t stress this enough. If you have PAD, inspect your feet daily for any cuts, sores, or changes in color. Because of the reduced blood flow, even a small blister can become a serious problem. Wear comfortable, well-fitting shoes to prevent injuries.
September is a great time to schedule an appointment with your doctor to discuss your vascular health. It’s also an excellent opportunity to help spread the word among your friends and family. PAD is a serious condition, but with awareness and proactive care, we can help people live healthier, more mobile lives and prevent the devastating consequences of this disease.
Joe Altepeter, DPM, AACFAS, is a Podiatrist at Family Foot & Leg Centers in Fort Myers FL. He is a Fellow of the American College of Foot & Ankle Surgeons. Call 239-430-3668 or visit www.NaplesPodiatrist.com to make an appointment. Visit FootHealthFacts.org to learn more about foot and ankle conditions.
Disclaimer: This content is not intended to be a substitute for professional medical advice, diagnosis, or treatment. Always seek the advice of your physician or other qualified health care provider with any questions you may have regarding a medical condition.







