 Breast cancer is the number one cancer diagnosis among women in the United States and is second only to lung cancer in regards to cancer deaths. One in eight women, or 12.7%, will develop invasive breast cancer in her lifetime.
Breast cancer is the number one cancer diagnosis among women in the United States and is second only to lung cancer in regards to cancer deaths. One in eight women, or 12.7%, will develop invasive breast cancer in her lifetime.
Last year, an estimated 232,000 people were diagnosed with invasive breast cancer and approximately 39,000 died of breast cancer last year. The good news is, the number of these deaths is steadily decreasing. Medicine is making great strides against the disease thanks to early detection and better treatments.
Although the deaths are declining, these numbers are still alarming. Like any health ailment, you should be proactive and do anything you can to lower your risk of developing cancer. Risk factors are anything that increases your chances for developing cancer. Having a risk factor does not mean that you will develop breast cancers; some women with one or more risk factors never develop breast cancer. However, knowing the risk factors and how they affect you can help minimize your chances of developing breast cancer. You can control things like your weight, diet, alcohol consumption and smoking habit. On the other hand, risk factors such as: gender, age, family history, race, and density of breasts are those that you cannot control. One additional risk factor that you may not even know you have unless you are tested is a genetic mutation.
GENETIC RISK
Approximately 5 to 10% of breast cancers are thought to be hereditary or due directly from a mutation on a gene passed on from either your father or mother. Most inherited cases of breast cancer are associated with two abnormal genes: BRCA1 (BReast CAncer gene 1) and BRCA2 (BReast CAncer gene 2).
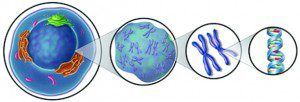
Everyone has BRCA1 and BRCA2 genes. The function of these genes is to repair cell damage and keep cells growing normally. BRCA1 and BRCA2 are human genes that belong to a class of genes known as tumor suppressors. When these genes contain abnormalities or mutations, they do not function normally and breast cancer risk increases.
Abnormal BRCA1 and BRCA2 genes may account for up to 10% of all breast cancers, or one out of ten cases. Having an abnormal BRCA1 or BRCA2 gene does not mean you will be diagnosed with breast cancer, but it does increase the chances of development.
The average American woman has a one in eight, or 12 to 13% chance of developing breast cancer in her lifetime. Women who have an abnormal BRCA1 or BRCA2 gene (or both) can have up to an 80% chance of being diagnosed with breast cancer during their lifetime.
Women with abnormal BRCA1/BRCA2 genes also have an increased risk for developing ovarian, colon, pancreatic and thyroid cancers, as well as melanoma. Are your BRCA1 and BRCA2 genes abnormal, increasing your risk for developing breast cancer?
GENETIC TESTING
There are various genetic tests available to determine if someone has an abnormal BRCA1/BRCA2 gene. Several methods are available to test for BRCA1 and BRCA2 mutations. Most of these methods look for changes in BRCA1/BRCA2 DNA. At least one method looks for changes in the proteins produced by these genes. Frequently, a combination of methods is used.
A blood sample is needed for these tests. The blood is drawn in a laboratory, doctor’s office, hospital, or clinic and then sent to a laboratory that specializes in the tests.
A positive test result generally indicates that a person has inherited a known harmful mutation in BRCA1 or BRCA2 and, therefore, has an increased risk of developing breast cancer.
ABNORMAL BRCA GENES – NOW WHAT?
Several options are available for managing cancer risk in individuals who have a harmful BRCA1 or BRCA2 mutation. If you do have an abnormal gene, there are lifestyle choices you can make to keep your risk as low as possible. These include:
. Maintaining a healthy weight.
. Exercising regularly.
. Limiting alcohol.
. Eating nutritious foods.
. Never smoking or quit if you do smoke.
These are just a few steps you can take to lower your chance of developing cancer. Along with these lifestyle choices, there are other risk reduction options for women at higher risk because of abnormal genes.
If you are at higher risk because of an abnormal breast cancer gene, you and your doctor will develop a screening plan tailored to your unique situation. It may be determined that you should begin regular screenings before the generally recommended age of 40. In addition to the screening guidelines for women at average risk, a screening plan for a woman at high risk may include:
. Monthly self breast examination.
. Yearly breast examination by your doctor.
. Digital mammogram every six months or every year starting at the age of 30 or younger.
. Breast ultrasound every six months or every year.
. MRI breast screening every year.
Besides close surveillance, there are other ways to minimize risk if you have abnormal BRCA genes including: research trials, medications, and prophylactic or preventative mastectomy or oophorectomy. Talk to your doctor, radiologist or genetic counselor about developing a specialized program for early detection that addresses your breast cancer risk, meets your individual needs and gives you peace of mind.
Check-in Express – hold your place in line without sitting in the waiting room.
This service is free for patients to use. Simply text the code for the center you wish to visit (2273 for Estero and 3333 for Cape Coral) to 239-330-2654, answer a few short questions via SMS text, and we will automatically confirm that we are holding your place in line.









