By John Canterbury, M.D.
 This past September, federal health officials declared they had “potentially lifesaving information.” The information they were referring to was pertaining to a major blood pressure study. They ended the study more than a year ahead of schedule because they conclusively answered a question cardiologists have puzzled over for decades: How low should blood pressure go?
This past September, federal health officials declared they had “potentially lifesaving information.” The information they were referring to was pertaining to a major blood pressure study. They ended the study more than a year ahead of schedule because they conclusively answered a question cardiologists have puzzled over for decades: How low should blood pressure go?
According to the study, the answer: it is safe and possibly lifesaving for blood pressure to be considerably lower than current guidelines.
For years doctors have been uncertain what the optimal goal should be for patients with high blood pressure. The aim, of course, is to bring it down but how far and how aggressively remained a mystery. There are trade-offs — risks and side effects from drugs — and there were lingering questions about whether older patients needed somewhat higher blood pressure to push blood to the brain.
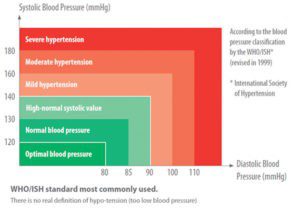
The study found that patients who were assigned to reach a systolic blood pressure goal below 120 — far lower than current guidelines of 140, or 150 for people over 60 — had their risk of heart attacks, heart failure and strokes reduced by a third and their risk of death reduced by nearly a quarter.
The study, called Sprint, randomly assigned more than 9,300 men and women ages 50 and over who were at high risk of heart disease or had kidney disease to of two systolic blood pressure targets: less than 120 millimeters of mercury, which is lower than any guideline ever suggested, or less than 140. (Systolic pressure is the higher of the two blood pressure numbers and represents pressure on blood vessels when the heart contracts.)
The study was expected to conclude in 2017, but considering the results of great importance to public health, the National Heart, Lung and Blood Institute announced, in September, saying a paper with the data would be published within a few months.
Many physicians agree that the findings from this study may provide potentially lifesaving information for patients with high blood pressure.
Nearly 79 million adults in this country — one of three — have high blood pressure, and half of those being treated for it still have systolic pressures over 140.
Much like previous studies on lowering cholesterol, physicians predict that this study will change they way blood pressure is treated. Contrary to what most people had thought about blood pressure for years, now it is believed that the lower the number the better.
If guidelines are changed because of this study — as blood pressure experts expect that they will be — an already falling death rate from heart attacks and stroke could drop even more.
Because cardiovascular disease is still the leading cause of death in the United States, a change in blood pressure goals could also reduce the nation’s overall mortality rate.
The study ventured into unknown territory that some had found a bit frightening. A systolic pressure that is naturally 120 might be good, but it is quite another matter to artificially drag pressure down so low with drugs.
Reaching a target that low would mean giving people more and more medications, and the side effects could cancel any benefit. Older people might be especially vulnerable to ill effects of a much lower blood pressure since many already take an array of drugs for chronic conditions, which might interact. A very low blood pressure could lead to dizziness and falls. Twenty-eight percent of the subjects in the new study were over age 75.
Less than two years ago, a National Heart, Lung and Blood Institute panel went in the opposite direction. People had been told to aim for a systolic blood pressure of 140. But the panel recommended a goal of 150 for people ages 60 and older, arguing that there were no convincing data showing lower is better.
Until now, many blood pressure experts thought they were doing about as well as possible. The incidence of strokes — the major consequence of high blood pressure — has fallen by 70 percent since 1972. The main problem was that so many patients with high blood pressure did not take their medications or took drugs that were not powerful enough.
It was not always easy for people in the study to reach their blood pressure goals. Those assigned to get their pressure below 140 took, on average, two drugs. Those assigned to below 120 took an average of three drugs. Cost usually is not an issue for high blood pressure patients because 90 percent of blood pressure drugs are available as generics.
The study also asked whether a lower blood pressure would help people with kidney disease and whether people would think more clearly and have less dementia. That was one hypothesis, but it also was possible that a lower pressure would mean less blood gets to the brain and kidney, with detrimental effects. The results of a lower blood pressure on the kidneys and the brain are still being analyzed.
People with high blood pressure should not panic. They do not need to rush to their doctors asking to suddenly change medications. High blood pressure takes its toll slowly. No one is in imminent danger. If your physician thinks it is best for your medications to be increased or changed in any way, they will inform you when the time is right.
If you have any questions about the current blood pressure guidelines or would like to learn more about how to lower and maintain your blood pressure, speak with your primary care physician.
John Canterbury MD
South Florida Internal Medicine
680 Second Avenue North, Suite 203
Naples, FL 34102
239-330-1382
*courtesy of New York Times









