By Prathima Moorthy, M.D. –
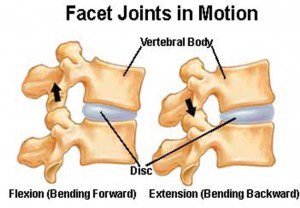 Cervical facet syndrome is a cause of pain in the spinal region and, more noticeably, in the neck. The facet joints are what connect the vertebrae in the spine. They are joints, like others in your body, which allow your spine to move in different directions. Because of the constant motion, they can become worn or torn.
Cervical facet syndrome is a cause of pain in the spinal region and, more noticeably, in the neck. The facet joints are what connect the vertebrae in the spine. They are joints, like others in your body, which allow your spine to move in different directions. Because of the constant motion, they can become worn or torn.
Symptoms of Cervical Facet Joint Disease (Osteoarthritis)
When suffering from cervical facet syndrome, the facet joints become inflamed and may bring with it neck pain, soreness and or stiffness. Cervical facet joint pain can be felt in the areas of the base of the skull, upper back and shoulders, mid-back or neck. In many cases, cervical facet syndrome is the cause of trauma from an injury to the facet joint, due to a degenerative disc disease or also due to stress or strain in your posture.
Individuals suffering from cervical facet syndrome usually feel worse in the morning. They tend to have stiffness and usually will feel somewhat better after they have been moving around. As the day progresses, they tend to be ok as long as they keep moving. However, for those having to work seated all day or work from a computer, they may find they are at greater risk of experiencing pain throughout the day.
Sufferers of cervical facet syndrome often have problems with headaches as well. Pain may be felt in different areas and usually when moving the head in up and down movements. Headaches are less of an issue with joint problems in this area, however, stiffness of the neck and tightness and pain in the shoulder area is present. Neurological symptoms, such as numbness and muscle weakness, are also factors of cervical facet joint disease. Patients often experience headaches and neck pain, and a dull, aching, uncomfortable feeling in the back of the neck that may move, or radiate, to the shoulder and middle of the back.
Initial Treatment for Cervical Facet Syndrome
Physical therapy is one method which can help reduce the pain by using ice to decrease the blood flow to the injured area and can also alleviate any spasms which may occur. The use of ultrasound, electrical stimulation, muscle relaxants and non-steroidal anti-inflammatory medication can also be used effectively to reduce the pain.
What Causes the Cervical Facet Joints to Become Painful?
Osteoarthritis is probably the most common cause of cervical facet joint pain. This degenerative disease causes progressive cartilage deterioration. Without the spongy cartilaginous cushion, joint bones begin to rub against each other when at rest and during movement. Another condition, Degenerative Disc Disease (DDD) may compromise the structural integrity of the intervertebral discs causing discs to lose normal height. Loss of disc height may cause the affected facet joints to become positioned too closely thereby disrupting the joint’s ability to function normally.
Diagnosis of Facet Joint Problems
The most definitive diagnosis of facet joint pain can be made by a facet joint block. This is an injection with a small volume of a combination of local anesthetic and cortisone used to block the nerve that innervates the facet joint. If a patient experiences significant pain reduction from this procedure, he or she may be a candidate for a Radiofrequency Ablation procedure. This is a minimally-invasive procedure available to diagnose and aid in treatment of cervical facet syndrome. The benefits of having this type of surgery vs. conservative surgery include, but are not limited to: no general anesthesia; no hospital stay; and a quick recovery that results in the patient being able to resume their normal lifestyle in a minimal amount of time.
How Can Radiofrequency Ablation (RFA) Relieve Symptoms?
RFA is a minimally-invasive procedure that disables and prevents a specific spinal nerve from transmitting pain signals. It was developed more than 30 years ago and is performed by many pain management specialists to treat painful facet joints. RFA applies a precisely targeted electrical field to change the function of nerves – in this case, a specific branch of a spinal nerve rendering it incapable of transmitting pain signals.
What are the Possible Complications with RFA?
As with any medical procedure, there are risks and potential complications. Although complications rarely occur, patients need to know what could happen. The following list is not conclusive: bleeding, infection, nerve or injury, allergic or other reaction to medications used (e.g. anesthetic).
Is the Pain Relief Permanent?
For many patients who suffer chronic neck pain, RFA is an effective treatment that may provide relief for six months or longer. Even when normal function returns to the target, pain relief may continue. If the patient responded well to the first RFA, a second may be considered if pain resumes. Of course, each patient is unique and what works well for one person, may not work well or at all for another.
How is the Procedure Performed?
Using gentle heat through the needle, the physician can cause muscle twitches or tingling sensations that confirm that the needle is properly and precisely positioned next to the targeted spinal nerve branch. Electric energy is then applied for the next 90 seconds to “ablate” the nerve. This procedure is repeated for each targeted nerve root. In general, there is minimal pain with this procedure.
What Should Patients Expect?
Like other minimally-invasive outpatient procedures, some post-procedural pain or discomfort should be expected. Usually an over-the-counter NSAID is sufficient to relieve this discomfort. In some cases, post-procedural pain may increase and the physician will prescribe needed medication (e.g. anti-inflammatory).
In general, patients can expect a significant reduction of their pre-procedural pain in one to four weeks. It is recommended that before deciding on the appropriate form of treatment, that you explore all options and treatment procedures available to you.
Prathima Moorthy, M.D. | 239-593-9594 | Pain Management Center of Naples | 3439 Pine Ridge Rd., Naples, FL 34109









