By Carol DiNicolantonio R.Ph.
 The Framingham score assesses a patient’s risk of a coronary heart disease (CHD) event (like fatal or nonfatal MI) over 10 years. The Framingham underestimates the life time risk especially in the youth and in women.
The Framingham score assesses a patient’s risk of a coronary heart disease (CHD) event (like fatal or nonfatal MI) over 10 years. The Framingham underestimates the life time risk especially in the youth and in women.
In people with CMR (cardio metabolic risk) defined by lipoprotein abnormalities; increased Triglycerides (TG), low High Density Lipoproteins (HDL) and increased small dense Low Density Lipoproteins (LDL) particles. CMR characteristics include central obesity, insulin resistance, dyslipoproteinemia, and hypertension. The primary objective in reducing Cardio Vascular Disease (CVD) events is to lower LDL which has been demonstrated to reduce risk of Coronary Heart Disease (CHD) and Stroke.
Apolipoprotein (ApoB) and LDL particle size are more reliable predictors vs. LDL or non-HDL when it comes to on-treatment residual CVD risk. Increased TGs are moderately associated with an increased CVD risk, especially in women. Decreased TGs and increased HDL are secondary levels of importance compared to LDL.
The preferred agent to use with a statin drug (Crestor ®, atorvastatin, lovastatin and simvastatin) to increase HDL is niacin because there is better evidence for reduction in CVD events as mono or combination therapy vs. fibrates. Fibrates (fenofibrate) have been shown to reduce CVD events but not mortality. In the FIELD and WHO trials, and the VA-HIT (with Gemfibrozil). Fenofibrate was shown to reduce non-fatal Myocardial Infarction (MI) which is a heart attack in laymen terms, significantly but it caused a non-significant increase in fatal MI in the FIELD study.
Both TZDs increase LDL particle size. Actos® – Increases HDL more vs. Avandia®, and Actos®, lowers TGs where Avandia®, increases TGs. Also Actos® lowers LDL particle number whereas Avandia®, increases LDL particle.
Atherosclerosis is present in up to 40-50% of women and men by the age of 50. CHD risk is more directly related to the number of atherogenic lipoprotein particles vs. the total volume of LDL.
A normal LDL could be measured in someone with an extremely atherogenic level of small, dense LDL particles. Each LDL particle contains a single apolipoprotein (apoB) therefore measuring apoB provides a direct measurement of LDL particles, but not the LDL particle make up (small dense LDL vs. larger buoyant LDL). There is clinical evidence that measuring apoB is superior to measuring LDL for predicting probability of fatal and nonfatal CHD.
Statins reduce LDL content more than LDL particle concentration whereas fenofibrate reduces LDL content less versus LDL particle concentration, which could explain why so many people on optimum statin therapy will still experience CHD events. Assessment of apoB has been recommended for all guidelines as an indicator of cardiovascular risk.
Major CVD risk factors are Smoker, family history of premature CAD, hypertension.
Questions: what’s considered family history of premature Coronary Artery Disease (CAD) and does hypertension mean uncontrolled hypertension or anyone on a medication for hypertension even if they are controlled or just if they’re uncontrolled?
Diabetic patients usually have different LDL particles versus the normal population.
1. Non-HDL cholesterol levels (TC-HDL = concentration of cholesterol within all lipoprotein particles considered atherogenic, tending to promote the formation of fatty plaques in the arteries) and has been demonstrated to be a better predictor of CVD vs. LDL especially in statin patients and is a secondary goal of therapy after LDL in the ATPIII guidelines in people with hypertriglyceridemia (TG > 200) or metabolic syndrome. Non-HDL is a better predictor due to the fact that LDL-C underestimates the burden of atherogenic lipoprotein. Also non-HDL cholesterol adds no additional cost and it is easy to calculate (Total Cholesterol – HDL).
You can determine if someone has subclinical vascular disease by measuring coronary calcification, carotid intima-media thickness, or the Ankle-Brachial Index (ABI-Index). Someone who smoked for many years is more likely to have smoking related arterial lesions.
Statins, fibrates, niacin bile acid sequestrants (gemfibrozil) as mono-therapy have all been shown to decrease CV events in clinical trials but the incremental benefit in combination therapy still is in question.
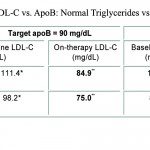
In diabetic patients on statin therapy, in order to achieve an ApoB = 90 it required an LDL-C of 82.5 and in non-diabetic patients it required an LDL-C of 80.4. 82.5 and 80.4 are significantly lower than the suggested LDL-C target of < 100 and according to these results it is reasonable to lower a patient’s LDL-C to < 85 if their goal is an LDL-C of < 100.
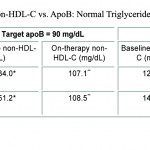
Also in order for diabetic and non-diabetic patients to achieve an ApoB level = 90 it required a non-HDL-C (mg/dl) of 108.7 and 106.5 respectively. Thus the goal for a non-HDL-C of < 130 may need to be lowered to < 110 especially if the patient is going to hit a goal of ApoB < 90.
Table 4. Linear Regression of LDL-C vs. ApoB: Normal Triglycerides vs. High Triglycerides
These data support that diabetics or patients with high triglycerides should be treated to an LDL-C of < 70 mg/dl, non-HDL-C < 100 mg/dl, and apoB < 80 mg/dl.
In summary if you get the patient’s LDL-C to 70 mg/dl and non-HDL-C to 100 mg/dl, the patient’s apoB will be less than 90 and pretty close to 80 mg/dl. Also people with diabetes or without diabetes require lower LDL-C and non-HDL-C goals to get their apoB to the recommended level. If you can’t measure apoB then look at non-HDL-C since it is correlated better with apoB versus LDL-C.
Regardless of race or ethnicity, LDL-C and non-HDL-C need to be close to the currently recommended goals for very high-risk CHD patients in order for them to achieve apoB goals.
At Home Medication Review
Carol DiNicolantonio R.Ph.
(716) 310-9144