By Debra K. Brinker, RN
The majority of us will suffer from a condition associated with back pain at some point in our lives. A common misconception is that if you have pain, you should first get an MRI and a surgical consultation. But back pain should not be an automatic indication that these drastic steps are necessary. The body has fantastic regenerative capabilities that can, with the right stimulus, strengthen and repair the pain-causing structures without surgery.
Pain after back surgery
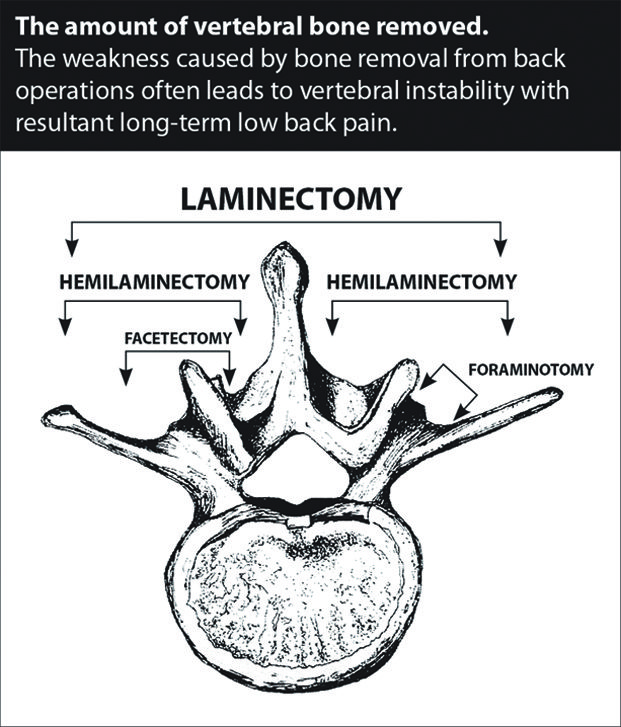
Why do some patients continue to experience pain after undergoing surgery? The underlying problem was not addressed, or may have been worsened, during surgery. In order to see and access the vertebrae, discs, and lamina the surgeons need to first cut through the surrounding soft tissue, weakening the stabilizing anatomy. Throughout the surgery, more tissue is cut, scraped, and/ or removed. (See figure 1.) Afterward, the balance, function and motion of the entire vertebral joint structure changes, stressing and injuring new areas. This off-balance joint will degenerate faster than a non-surgerized joint. In one study, researchers compared patients who had a first-time lumbar discectomy to those who received conservative care. The results showed the lumbar discs of the standard discectomy group degenerated at a 47.6% faster rate over the first 2 years and 95.2% over the next 6 years. That is a striking illumination of what lies ahead after this surgery… degeneration. As these discs wear out further, an operation to fuse together the adjacent joints, in an attempt to relieve the new or continued pain, may be undertaken.
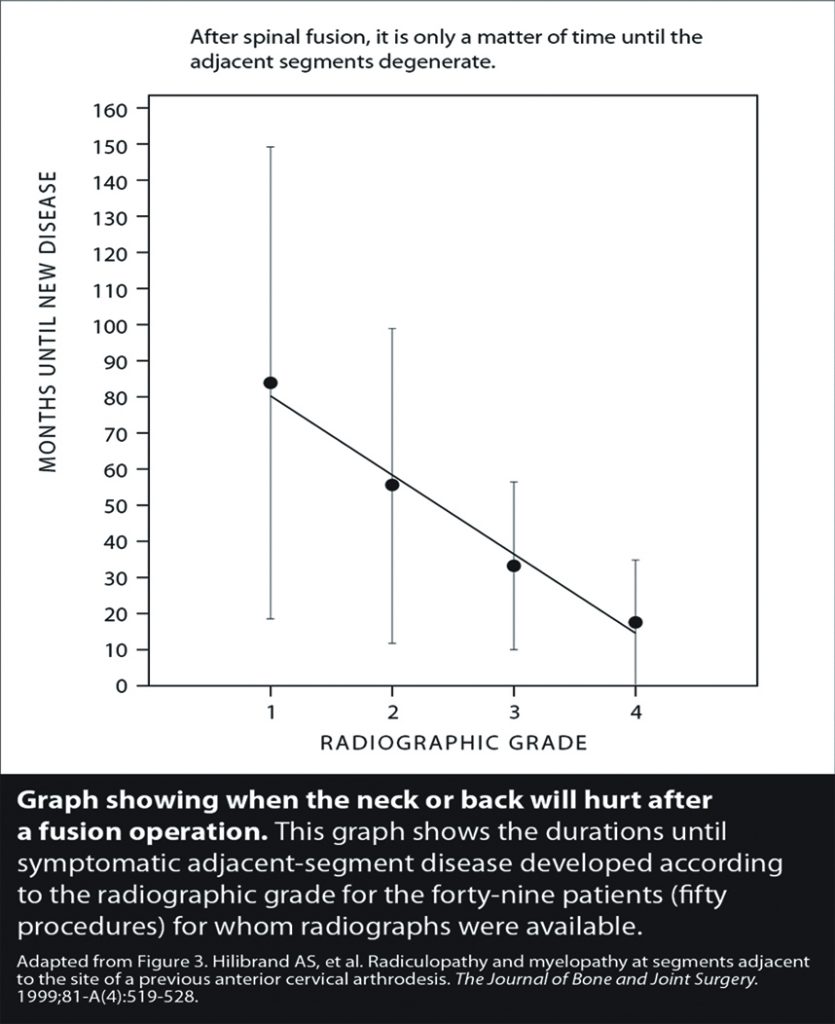
Spinal fusion permanently fuses together segments of the vertebrae. The fusion limits mobility and can cause back pain, especially when trying to bend. While fusion surgery is necessary in some more severe cases, it is important to understand the long-term consequences as it relates to adjacent segment disease. Fusion changes the mechanics of the vertebral segments, causing stress at the areas above and below the fusion and increasing intradiscal pressure, which leads to the continued breakdown of the spine. It is only a matter of time before the adjacent segments cause pain. (See figure 2.)
Sadly, even more than a year following fusion surgery, over half of patients who received the procedure continue to chronically use opioid painkillers. Pain continues in far too many patients long after the surgery!
Spinal instability is a commonly missed diagnosis prior to surgery
Joint instability due to ligament laxity is the cause of most chronic pain, including low back pain. Degeneration of a disc begins as soon as the lumbar ligaments become loose and cause spinal instability. Healthy ligaments hold adjacent bones together, and are the major stabilizing factor in the lumbar spine. Injured and weak ligaments (from trauma, wear and tear, or surgery) allow the vertebral segments to move excessively and cause pain. The excessive motion between the vertebrae increases the strain on the discs, and the increased pressure causes them to degenerate and possibly to herniate. (See figure 3.)
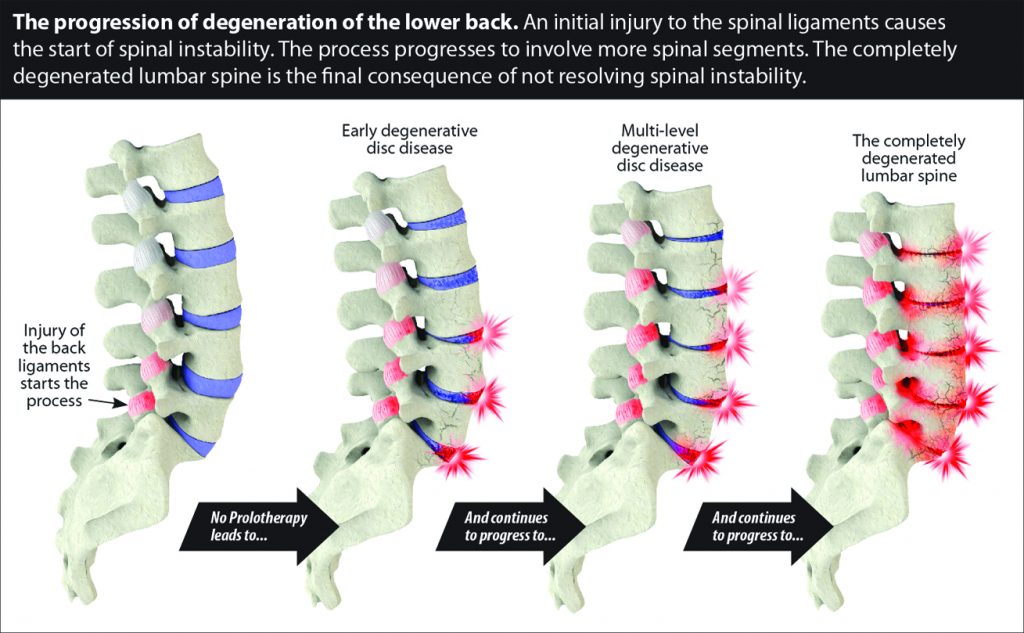
These flattened and herniated discs are unable to provide the same cushion, which makes the lumbar ligaments work even harder. The muscles also have to work harder, often resulting in added tension and spasms. Add to this the use of repair-inhibiting anti-inflammatories (such as NSAIDs and corticosteroids), and thus continues the downward spiral of pain!
It is important to understand that pain is an indication of tissue damage. (See figure 4.)
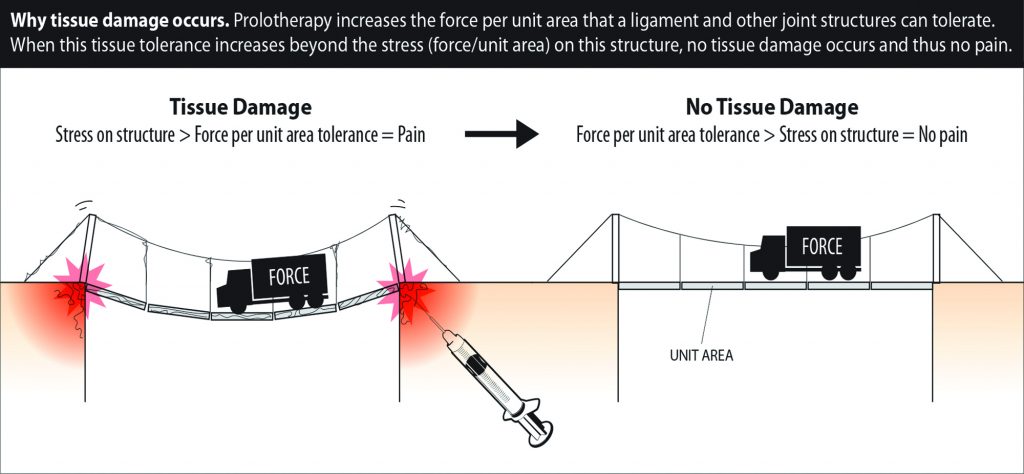
This means that there was tissue damage present prior to surgery, and afterward, there was still damage, or even more. Standard conservative care such as massage and physical therapy focus on muscle work and often provide short-term relief of symptoms such as muscle spasms, or help to correct posture and encourage exercise, which are helpful, but they do not induce the necessary long-term repair of the ligamentous source. The muscles are used to move joints, but are not meant to be the primary stabilizers—that job is meant for the ligaments.
Regenerative treatments are capable of resolving many back pain conditions with underlying spinal instability by strengthening the vertebral ligaments, stabilizing the spine, and preventing the progressive degeneration that occurs to the intervertebral discs. Unfortunately, patients often seek this method of treatment after they have already failed back surgery, rounds of steroid injections and conservative care, in an effort to alleviate the unending pain cycle. Seeking regenerative options sooner in cases of back pain or when diagnosed with a degenerative condition can help stop the pain cycle earlier and potentially avoid the post-surgical pitfalls.
Regenerative Medicine Specialists
CaringMedical.com
239-303-4546
with locations in Fort Myers and Chicagoland
1 Schroeder JE, Dettori JR, Brodt ED, Kaplan L. Disc degeneration after disc herniation: are we accelerating the process? Evidence-Based Spine-Care Journal. 2012;3(4):33-40. doi:10.1055/s-0032-1328141.










