Improve Cures Rates and Reduce Side Effects
– By John Sylvester, M.D. –
 Prostate Cancer is the most common cancer (other than skin cancer) in men. Over 200,000 men are diagnosed each year in the USA. The death rate has dropped over 40% over the past 20 years thanks primarily to early detection from PSA screening. Medical journals publish 100’s of articles each year on the diagnosis, treatment and side effects of prostate cancer treatment. Treatment options are many and growing. It is not surprising that patients often feel overwhelmed when discussing their management options with their physician. In this short article I will review the latest advances in minimally invasive prostate cancer treatment.
Prostate Cancer is the most common cancer (other than skin cancer) in men. Over 200,000 men are diagnosed each year in the USA. The death rate has dropped over 40% over the past 20 years thanks primarily to early detection from PSA screening. Medical journals publish 100’s of articles each year on the diagnosis, treatment and side effects of prostate cancer treatment. Treatment options are many and growing. It is not surprising that patients often feel overwhelmed when discussing their management options with their physician. In this short article I will review the latest advances in minimally invasive prostate cancer treatment.
The main options for patients with newly diagnosed, apparently localized (not metastatic) prostate cancer have been, and remain radiation therapy and surgery. Radiation therapy can be delivered by external beam radiation therapy (EBRT) and/or brachytherapy (LDR or HDR). Surgery, radical prostatectomy (RP) is usually done with robotic assistance in this country. There are advantages and disadvantages to each form of treatment. I’ll briefly discuss the success rate as defined by the patient’s PSA dropping to a very low number after treatment and remaining very low. This is called biochemical relapse-free survival (BRFS); it is the most sensitive measurement of success of a given treatment. I’ll also discuss the logistics of the various treatments and common temporary and possible long term side effects. All of this is based on what is actually published in peer reviewed medical journals.
We divide prostate cancer into low, intermediate and high risk disease based on pre-treatment PSA, biopsy Gleason score and digital rectal exam (DRE). One commonly used system is:
Low risk: PSA < 10, and Gleason score 20, Gleason 8-10, DRE T2c or T3 (or 2 or more intermediate risk factors).
The higher the risk-group the higher the chance microscopic prostate cancer is outside of the prostate (BJU 2013 updated Partin Tables) and less curable by surgery alone. Also the very high risk groups have a higher chance some cancer cells may have microscopically spread to the bone, lymph nodes or elsewhere. Microscopic means it cannot be seen on any type of scan (PET/CT, Bone Scan, MRI etc).
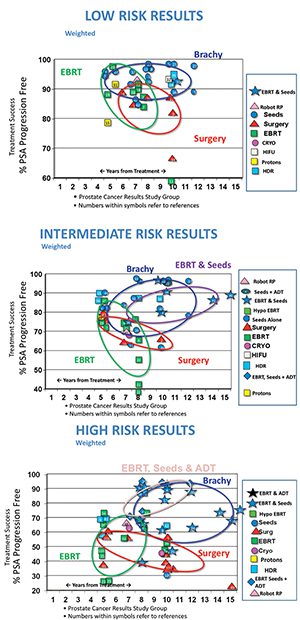
In General Low-risk prostate cancer has very high cure rates (BRFS) with surgery or radiation therapy, somewhat lower success rates with cryotherapy (freezing the prostate). The largest study ever published comparing BRFS outcomes between the various treatment options was first published in IJROBP Oct, 2009 (Grimm, Sylvester et al) then updated and published in BJU in 2012. See figures 1, 2 and 3. As one can see from the tables low risk disease has excellent BRFS outcomes with brachytherapy, IMRT and surgery, but as the risk groups move higher the surgical results fall and the combination of EBRT and brachytherapy (radioactive seeds) continue to show excellent long-term outcomes. If a patient has surgery for higher risk disease he may benefit from post-operative adjuvant radiation therapy (depending on final pathology results), which can result in excellent long-term BRFS outcomes too.
Surgery is a one-time procedure with a short hospital stay, one sees the final pathology, it has a long track record and excellent BRFS outcomes for low-risk and favorable intermediate risk patients. It has a very low risk of bowel toxicity, but a significantly higher risk of urinary incontinence and impotency than the radiation options. It is a major surgery with all the usual surgical risks.
The newest technology is robotic assisted prostatectomy which reduces blood loss and hospital stay, but has not been proven to improve cancer control rates or urinary and sexual side effects.
IMRT (EBRT) has the advantage of no surgical risks and also has excellent BRFS outcomes for all risk groups, often combined with brachytherapy and/or hormonal therapy in higher risk and higher tumor volume settings. It is Monday thru Friday ~ 5-15 minutes a day for 5 weeks (if combined with brachytherapy), 8 weeks (if after surgery), or 9 weeks (if no prior surgery or brachytherapy planned). Temporary fatigue and increased frequency and urgency of urination and bowel movements are common. The long term risk of incontinence and/or bowel problems are very low with modern technology. Risk of impotency is age and health related. The most advanced form of IMRT is Cone-Beam CT Image-Guided Intensity Modulated Radiation Therapy with a Rectal Balloon or CBCTIGIMRTWRB.
Proton Beam Therapy is a type of EBRT. It does not have better cancer control or less side effects than other forms of radiation therapy. In fact, some studies show it to have lower cancer control rates and higher bowel toxicity rates.
Brachytherapy (radioactive seed implants = LDR) is a one-time outpatient 45 minute procedure. Has excellent long-term (15+ year follow-up) BRFS outcomes (John Sylvester MD et al: IJROBP 2007 and 2011) in all risk groups. Seeds are usually combined with a short course of IMRT in intermediate and high risk group patients. More recent reports show even better outcomes (S. Frank, J. Sylvester et al Cancer 2011 ) 99.1 % BRFS in low-risk and favorable intermediate risk patients. Newest technology is the THINStrand a new seed that is 42% thinner than the standard seed and results in higher quality treatment and less side effects than the standard seed (J Sylvester Brachytherapy 2013, B Moran IJROBP 11/2012). Radioactive seeds have more temporary urinary obstructive symptoms than IMRT, but a very low risk of incontinence and bowel problems, and the lowest published risk of impotency of any treatment.
Cryotherapy destroys tissue through freezing. It kills healthy cells and cancer cells. It has proven especially useful in the treatment of locally recurrent prostate cancer. It is performed in the O.R. under anesthesia with ultrasound guidance. It has a high risk of causing impotency, a low risk of incontinence.
HIFU is high intensity focused ultrasound and is not FDA approved in the USA. Is typically not covered by insurance and has a significantly lower BRFS rate than surgery or radiation therapy (IMRT or Seeds). Usually requires a pre-op TURP and/or hormone therapy, and a catheter post-op. It is being studied at a few sites in the USA. Some unscrupulous doctors are known to treat patients with HIFU without even having biopsy proof of cancer, they claim an MRI scan and elevated PSA blood test is all they need.
IMRT = Intensity Modulated Radiation Therapy
IJROBP= International Journal Radiation Oncology Biology and Physics
BJU= British Journal of Urology
Dr. John Sylvester
Dr John Sylvester is A Radiation Oncologist with 21st Century Oncology in Bradenton/Sarasota, FL. Previously he was co-founder and Director of The Seattle Prostate Institute and Director of the Puget Sound Tumor Institute. He has published over 70 articles in medical journals on prostate cancer, and multiple medical textbook chapters. He is lead investigator in multiple prostate cancer trials. He co-wrote the American Brachytherapy Society Prostate Cancer treatment guidelines and The Prostate Cancer Treatment Book. He is a member of the American Brachytherapy Society (ABS), The American Society of Therapeutic Radiation Oncology (ASTRO), The AMA, The Florida State Medical Society, and the American College of Radiation Oncology.
Dr. John Sylvester completed both his Medical Degree and specialty training in Radiation Oncology at UCLA. He is board certified in Radiation Oncology by the American Board of Radiology. He was awarded the American Cancer Society Fellowship during his year as chief resident at UCLA. He began performing prostate brachytherapy with Dr. Blasko in 1987, and joined the Seattle team full time in 1988. Dr. Sylvester co-founded the Seattle Prostate Institute and served as the Director of Education and Training for 8 years. He ran the internationally renowned monthly program which trained more physicians in prostate cancer treatment than any other program in the world, and the highly regarded Annual Seattle Advanced Prostate Brachytherapy Conference. Dr. Sylvester was the Director of the Seattle Prostate Institute from 2006-2008. He was in charge of the ABS Fellowship rotation at the Seattle Prostate Institute, a highly competitive and desired Fellowship program for residents in Radiation Oncology throughout North America. These programs trained the lead genitourinary Radiation Oncologists at UCSF, Harvard, MDAH, UCLA, Univ. Chicago, Emory, Rush, Cleveland Clinic, Wake Forrest, Duke, Princess Margaret, British Columbia Cancer Agency, virtually all of the prostate brachytherapy programs in Australia, New Zealand, England, and South America. Until his move to Florida in 2010, he was the Chief Medical Officer of Proqura, an organization developed by the Seattle team, focused on improving the quality of permanent prostate brachytherapy throughout the world.
Over the past 2 decades, Dr. Sylvester has performed over 3700 prostate brachytherapy procedures. He has developed, and assisted in the development, of several technical improvements in the prostate cancer treatments including:
– How to better visualize the urethra during the procedure.
– How to optimally utilize R.A.P.I.D. strand.
– He was the first physician in the U.S. to use I125 Echo Seed, a more visible (on ultrasound) radioactive seed.
– He was the lead Seattle investigator in a gene therapy protocol for salvage of external beam radiation therapy failures.
– He initiated the image-guided intensity modulated radiation therapy (IG-IMRT) approach used at the Swedish Cancer Institutes’
Radiation Oncology centers, for more precise Intensity Modulated Radiation Therapy (IMRT) for prostate cancer.
– He treated the first patient in the world with the first commercially available Calypso 4-D real-time image guidance unit for prostate
cancer IMRT.
– He co-authored the white paper on Calypso 4-D IG-IMRT.
– He worked with Oncura/General Electric to help create THINStrand, a new seed that is 42% thinner than standard sized seeds
(less trauma) and is the first physician to use that new seed.
– He is the lead investigator in a multi-institutional protocol evaluating the quality of life outcomes of patients treated with IMRT plus
a Cesium seed implant boost.
– Dr. Sylvester worked with the lead Brachytherapists at MDAH and Princess Margaret Hospital on an updated brachytherapy
outcomes nomogram evaluation that invalidated inaccurate the MSKCC brachytherapy nomogram..
– He is the first physician in the USA to use SpaceOAR in IG-IMRT prostate cancer patients as part of a randomized FDA protocol
hoping to reduce side effects of treatment.
– He is one of the four clinicians who wrote the ABS guidelines used by prostate cancer radiation oncologists worldwide.
The above work has led Dr. Sylvester to being called upon to present at national and international conferences on prostate cancer on a regular basis including: the World Congress of Endourology (Holland), American Society of Clinical Oncology, Urologic Society of Australasia (Melbourne), and European Association of Urology Conference in Germany, GEC-ESTRO/WCB conferences in Europe, and multiple times at the Annual American Society of Therapeutic Radiation Oncology (ASTRO) Conference, the Annual ABS (American Brachytherapy Society) Conference, The Annual Scottsdale Prostate Cancer Symposium, and The Annual Seattle Prostate Institute Advanced Brachytherapy Conferences. He was chosen to debate prostate cancer treatment techniques at the 2011 ABS meeting.
Dr Sylvester recently moved to Sarasota and now is a member of 21st Century Oncology at the Lakewood Ranch Radiation Center in Bradenton, FL where he continues cutting edge research in both prostate brachytherapy and IG-IMRT.









